This case is divided into two separate hospitalizations about 9 months apart.
Part 1
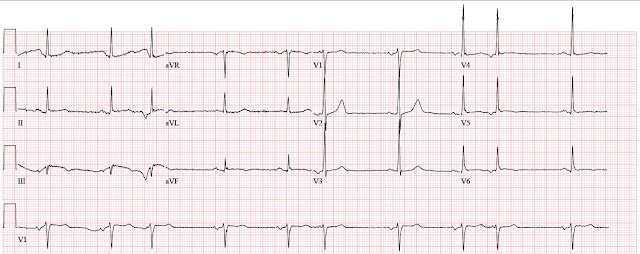
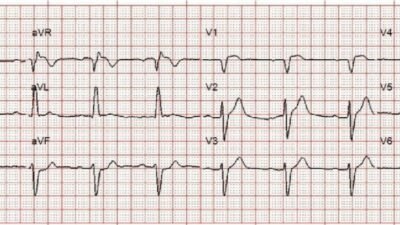
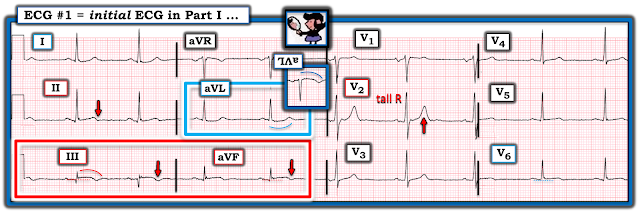
A man in his late 60s with hypertension, hyperlipidemia, type 2 diabetes mellitus, and a 50 pack-year smoking history presented at around 10 AM with acute onset chest pain which began several hours earlier while he was at home. He described it as a squeezing sensation across his chest radiating into the jaw. Before you see the ECG, you know the diagnosis.
- Nunes de Alencar J. Meyers HP. Frick W. McLaren J. Smith SW. Door-to-Balloon Time Outperforms ST-Segment Elevation in Predicting the STEMI vs. NSTEMI Final Diagnosis. Journal of Clinical Medicine 2025(14):6588. https://doi.org/10.3390/jcm14186588
Part 2
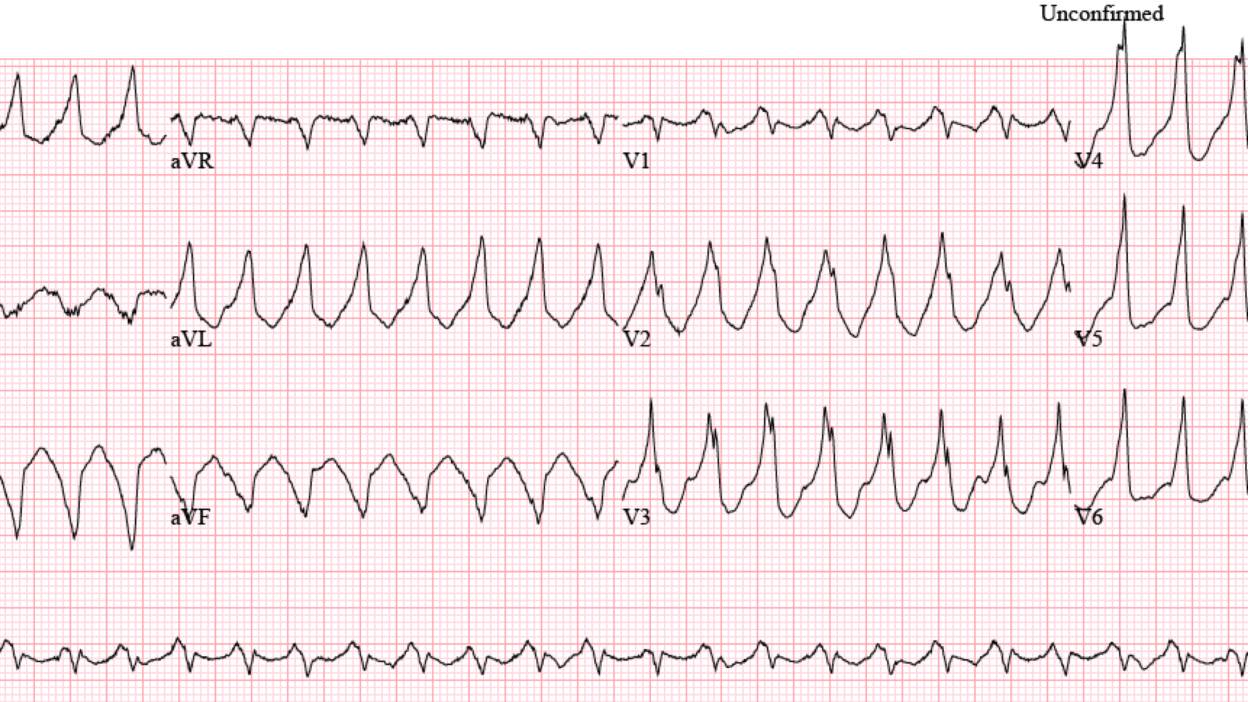
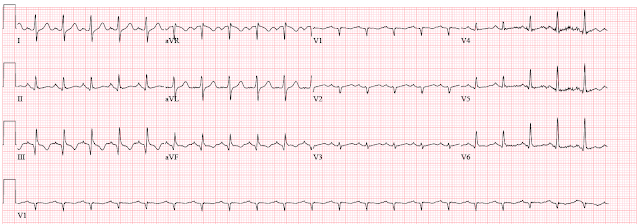
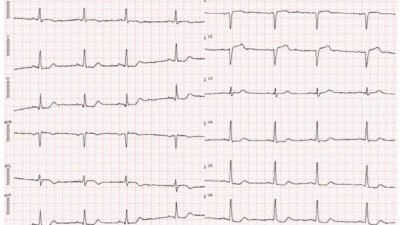
About 9 months later, the patient was admitted with sepsis secondary to complicated urinary tract infection. He has bladder cancer and obstructive uropathy which has been treated with percutaneous nephrostomy tubes. In addition, he had developed chronic HFrEF with EF 35% and inferolateral akinesis. While being monitored on telemetry, he developed salvos non-sustained ventricular tachycardia. The first ECG did not capture the VT.
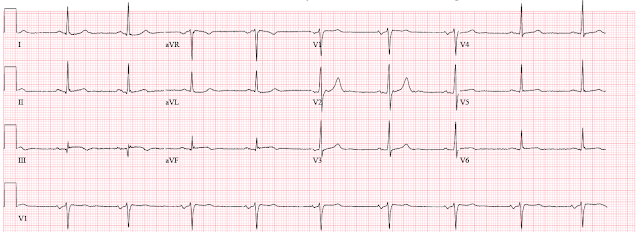
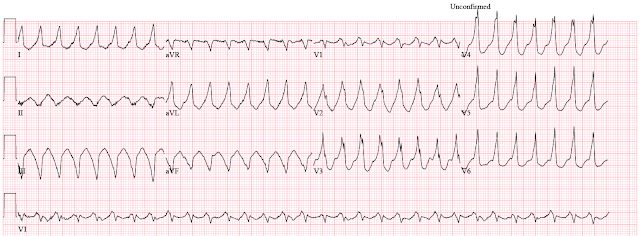
Sinus tachycardia (always worrisome) with old inferior infarct. The patient was reportedly resting comfortably in bed. Repeat ECG was performed during an episode of sustained ventricular tachycardia.
- First, the VT has a superior axis since it is originating from the inferior wall which is unlikely to be supplied by the LAD.
- Second, the VT is monomorphic which is likely scar mediated. The likelihood of an acute culprit in a patient with monomorphic VT and no ACS symptoms is very low.
Learning points:
- Quality improvement efforts consistently conceal missed OMIs, systematically biasing the literature and disguising shortcomings of the STEMI paradigm
- Monomorphic VT is usually scar mediated, not due to ACS
- First line treatment of electrical storm is amiodarone and propranolol, lidocaine is less effective
= = =
======================================
MY Comment, by KEN GRAUER, MD (10/21/2025):
Today’s 2-Part case by Dr. Frick contains much wisdom in his summarizing 3 powerful Learning Points. I focus my comment on a 4th essential Learning Point = The initial ECG in Part I of this case must not be interpreted as showing, a “nonspecific T wave abnormality”. Awareness of this point would have expedited the emergent cath that should have been done immediately after seeing the initial ECG in Part I of today’s case.
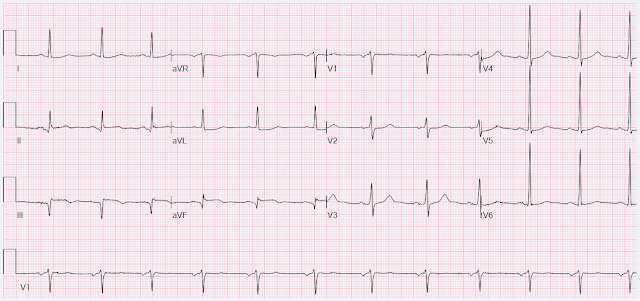
For clarity in Figure-1 — I’ve reproduced and labeled this initial ECG.
- The history is important. The patient in today’s case is a man in his late 60s, who presented in Part I with strong coronary risk factors and several hours of sudden and severe new CP (Chest Pain). As per Dr. Frick — regular readers of this ECG Blog knew the diagnosis even before seeing the initial ECG.
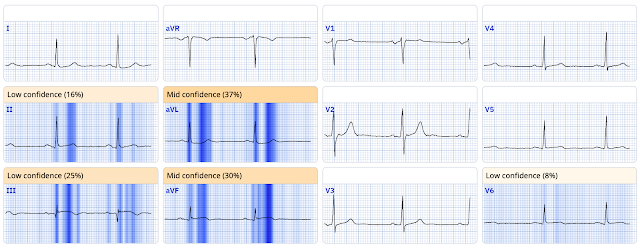
- As per Dr. Smith — there is no indication as to the presence or severity of CP at the time that ECG #1 was recorded. This historical information is critical, although it is all-too-often ignored. IF (as Dr. Smith suspects) this patient’s CP had decreased or resolved at the time ECG #1 was recorded — it would essentially confirm that this initial tracing represents an acute OMI that now shows reperfusion T waves. And because the “culprit” artery is in process of reperfusing — we are unlikely to find sufficient ST elevation to qualify as a STEMI.
- As a result of the preceding bullet — the 5th essential Learning Point in today’s post is that you are unlikely to see enough ST elevation to qualify as a STEMI if the patient’s acute OMI is in process of reperfusing. As a result — we need to stop looking for ST elevation in such tracings, and instead focus on the other ECG findings that confirm the diagnosis.
= = =
The Important ECG Findings in ECG #1:
As per Drs. Frick and Smith — ECG #1 is diagnostic of acute infero-postero-lateral OMI, now showing reperfusion T waves.
- My “eye” was immediately drawn to leads III and aVF (within the RED rectangle in Figure-1). There is ST elevation in both of these leads. The amount of ST elevation is not a lot in absolute measurement — but shape is more important than amount (albeit considering small size of the QRS in these inferior leads — the relative amount of ST elevation is considerable).
- The shape of the elevated ST segments in leads III and aVF is coved — and — the mirror-image opposite shape of the subtle-but-real ST depression in lead aVL confirms that this high-risk patient with several hours of new, severe CP has had an acute inferior OMI (ie, lead aVL clearly shows reciprocal ST-T depression that confirms acute inferior MI — this being the “magic” relationship between leads III and aVL with acute inferior MIs that we often refer to — as per My Comment in the June 10, 2025 — the May 10, 2025 and the July 11, 2018 posts, among many others).
- In addition — there is also T wave inversion in leads III and aVF, suggestive of at least some degree of reperfusion.
- Subtle supportive findings of the above findings are seen in lead II ( = the 3rd inferior Iead — with subtle hyperacute shape of its ST segment takeoff and a hint of beginning T wave inversion) — and — in lead I ( = the other high-lateral lead that shows a similar subtle coved ST depression as we see in lead aVL).
- Indication of acute posterior OMI — is forthcoming from the already tall R wave in lead V2, that manifests a taller-than-expected T wave following a longer-than-expected flattened ST segment — consistent with posterior reperfusion.
- There is no ST elevation in lead V5. But there is subtle ST elevation in lead V6, indicative of lateral OMI (shape being more important than the amount of this elevation).
- To Emphasize: The findings that I report in leads I, II, V2 and V6 are very subtle — and may not be appreciated by even experienced providers. But the diagnostic ECG findings of acute inferior OMI in leads III,aVF and lead aVL need to be looked for given the history in today’s case that, as per Dr. Frick — all-but-tells-us the diagnosis even before we see the ECG!
- 6th essential Learning Point — When we recognize several leads (such as leads III,aVF, aVL in today’s case) that we know are diagnostic of acute OMI — then IF we hone our attention looking for more subtle abnormalities — we will often find them in other leads, as we do here in leads I,II V2 and V6.
= = =
Figure-1: I’ve reproduced and labeled today’s initial ECG.
= = =