Written by Jesse McLaren, with edits from Smith
A 30 year old with a history of diabetes presented with two
days of intermittent chest pain and diaphoresis, which recurred two
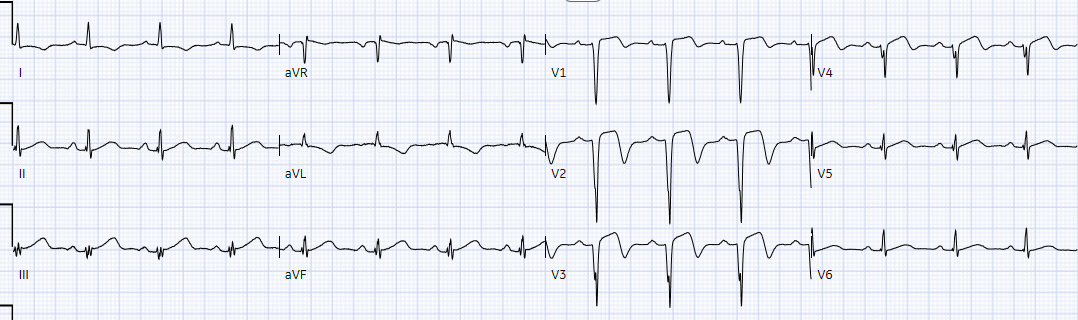
hours prior to presentation. Below is ECG #1 at triage. Are there any signs of
occlusion or reperfusion?
There’s normal sinus rhythm, normal conduction, normal axis,
normal R wave progression and normal voltages. There’s mild inferior ST
elevation in III that doesn’t meet STEMI criteria, but it’s associated with ST
depression in aVL and V2 that makes it diagnostic of infero-posterior Occlusion
MI (from either RCA or circumflex)– accompanied by inferior Q waves of unknown
age. There are also subtle biphasic T waves in V3-4 of unclear significance (this can be seen in anterior or RV reperfusion, but this usually does not accompany infero-posterior occlusion).
Just so you know this ECG interpretation is not done by the retrospectoscope:
I sent it to Dr. Smith without any information, and he immediately responded: “Infero-postero-lateral OMI”
The ECG had a computer and final cardiology interpretation
of “possible inferior infarct, age undetermined”, because of Q waves. It was
signed off by an emergency physician as “STEMI negative” because it did not
meet STEMI criteria. So the patient waited to be seen. First troponin I
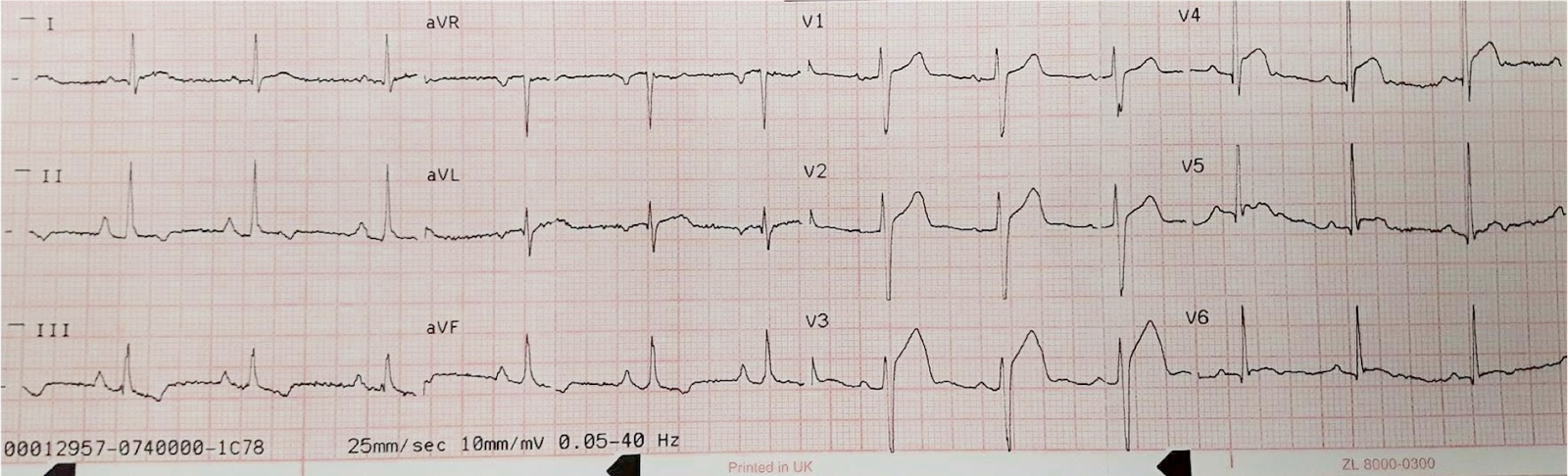
returned at 150 ng/L (<26 in males and <16 in females) and ECG #2 was
performed, with the patient painfree. What do you think?
Now the ST elevation in III with reciprocal change in aVL is
resolving, and V2 shows normalization of ST segment and slightly bigger T wave
– so there’s been infero-posterior reperfusion. And the biphasic T waves in V3-4
persist.
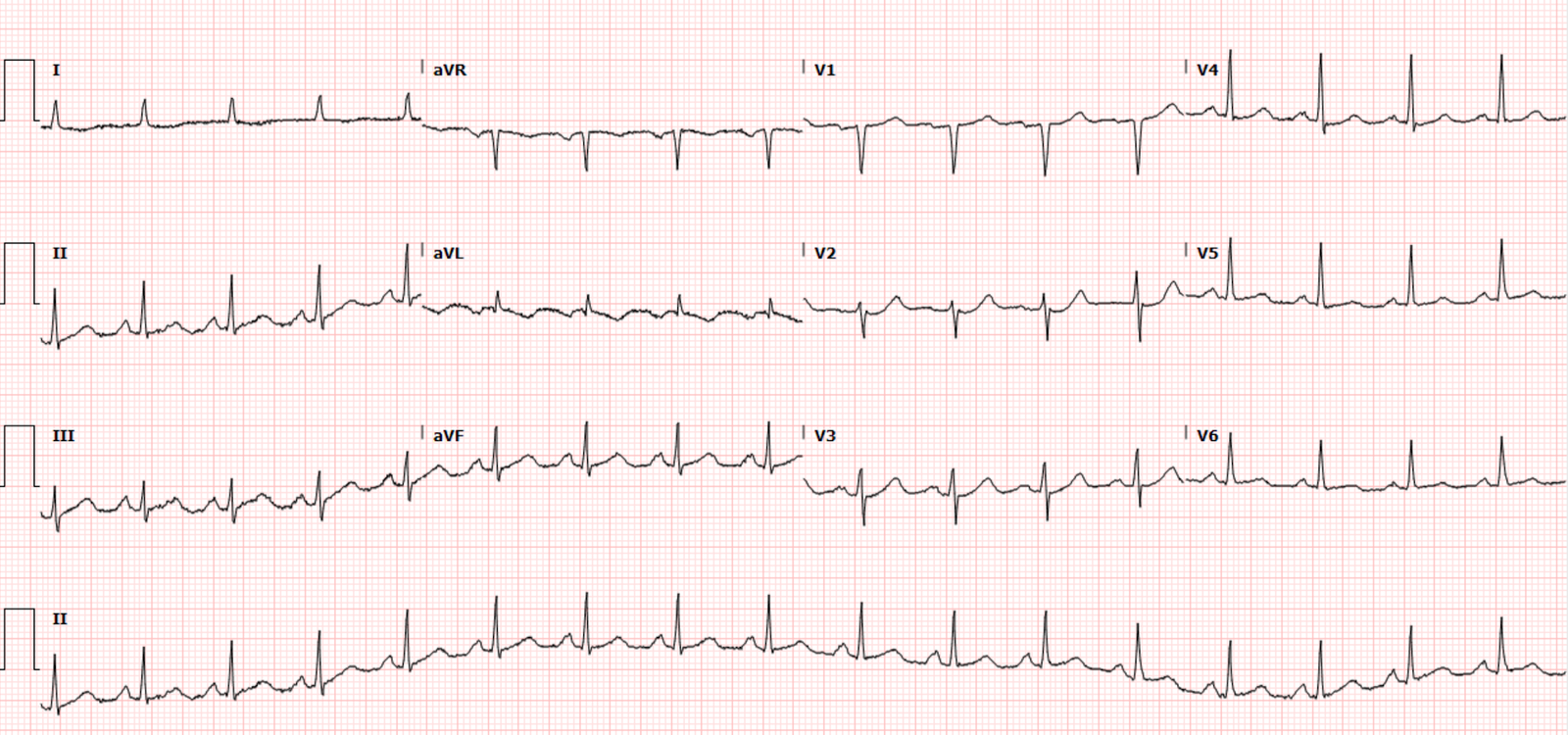
The patient was seen by an emergency physician 5 hours after
arrival, reporting no symptoms, with repeat trop down to 125 ng/L and ECG #3. What
do you think?
ST segment has risen again in III and there are bulkier
inferior T waves, with reciprocal ST depression in aVL and ST depression in V2.
But now there’s also been a loss of anterior R waves with new Q waves, and the
previously biphasic T waves in V3-4 are now upright (pseudonormalization). Moreover, T-waves in V3 and V4 are now bulky, suggesting they are hyperacute. So despite
a declining initial troponin and resolution of symptoms, the ECG shows reocclusion with OMI
affecting inferoposterior plus anterior walls. But it still doesn’t meet STEMI
criteria, so the patient was referred to cardiology as ACS.
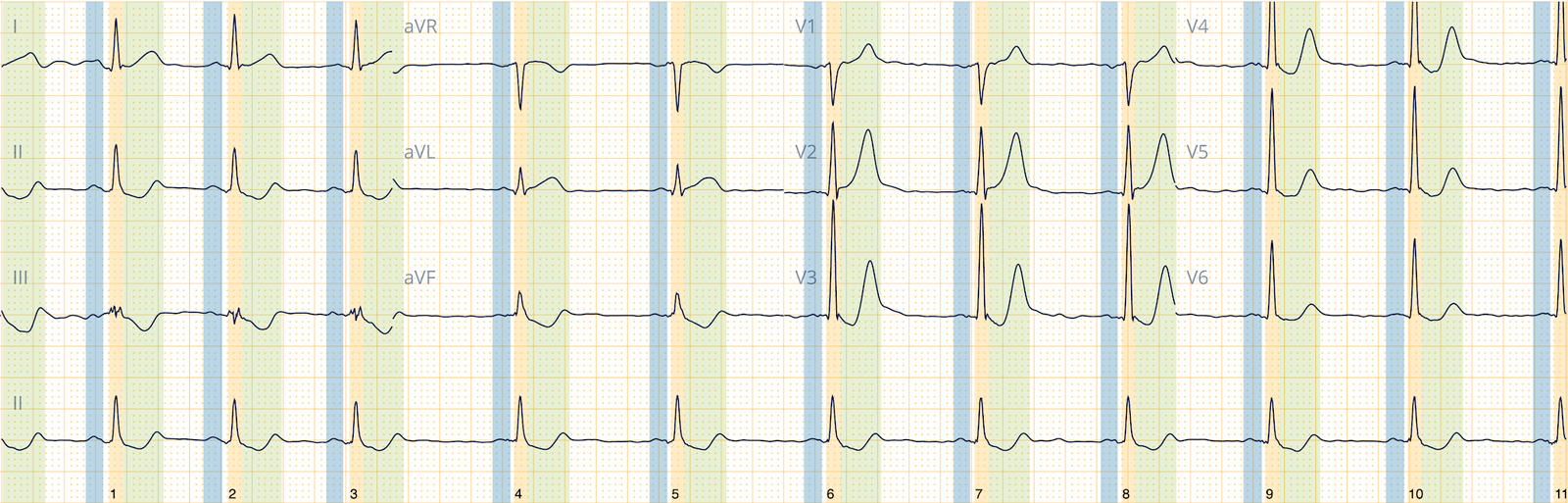
10 hours after arrival the patient was assessed by
cardiology and had ECG #4:
The ST elevation and reciprocal ST depression in aVL has
improved and T waves are no longer hyperacute. The transiently upright T waves
in V3-4 have inverted again, and now there’s T wave inversion across the
anterolateral wall. Now the main pattern is anterolateral reperfusion, most likely from proximal LAD
13 hours after arrival the patient complained chest pain and
ECG #5 was obtained, and repeat troponin was 11,000 ng/L.
There’s further loss of precordial R waves (in fact, profound Q-waves), with increasing
ST segment in V2 but ongoing reperfusion T wave inversion anterolateral. Recurring
symptoms suggest reocclusion, with an ECG between reperfusion and reocclusion. The
chest pain was refractory to nitro so the cath lab was activated: 100% proximal
LAD and 99% mid circumflex occlusions.
Peak troponin was 15,000 ng/L, and echo found preserved EF but
akinetic apex and hypokinesis of anterior and inferior walls. Next day ECG #6:
Evolution of LAD reperfusion with deeper T wave inversion anteriorly and aVL (with reciprocal taller T waves)
Discharge ECG #7 a few days later :
Ongoing
anterolateral reperfusion T wave inversion, with R wave recovery in V4-5 but
not V2-3.
Dual OMI, and dueling
OMI
STEMI is usually attributed to one infarct-related artery
that becomes completely and irreversibly occluded, producing regional ST
elevation that exceeds STEMI criteria. But this framework is proven to be
unreliable, and the underlying pathology of Occlusion MI is much more
complicated and dynamic: there can be little or no ST elevation but multiple
other signs of OMI, and this dynamic state can fluctuate between spontaneous
reperfusion and spontaneous reocclusion.
In addition, there are a number of other scenarios that
complicate OMI and ECG interpretation:
·
the occlusion of one infarct-related artery can
affect other territories based the site of occlusion. For example anterior and
inferior ST elevation can be caused by proximal
RCA or distal/wraparound LAD
occlusion
·
the occlusion of one infarct-related artery can
occlude collaterals that were serving another territory with chronic total
occlusion
·
the occlusion of one infarct-related artery can
induce subendocardial ischemia in another that had critical stenosis. For
example, inferior OMI with concomitant critical stenosis produces a combined
pattern (Aslanger’s
pattern) with inferior STE and subendocardial ischemia
·
occlusion of two infarct-related arteries simultaneously (“co-culprits”)
In this case there were two infarct-related arteries. This
complicated ECG interpretation because 1) there were two different patterns of
Occlusion, 2) neither of which ever met STEMI criteria, 3) they were
reperfusing/reoccluding at different times, and 4) had different effects on
some of the same leads. For example aVL is a high lateral lead which is
reciprocal to the inferior wall: inferior OMI can cause inferior ST elevation/hyperacute T with reciprocal ST depression in aVL (ECG #1/3), while lateral reperfusion can cause primary T wave inversion in aVL (ECG#4-7) with reciprocally tall inferior T wave. Similarly, the anterior lead V2 is reciprocal to the
posterior wall: posterior OMI can cause reciprocal ST depression in V2, while anterior reperfusion can cause primary T wave inversion in V2.
In other words, there was not only dual OMI, but they were
dueling – each going back and forth between occlusion and reperfusion, with
clashing ECG patterns that sometimes favoured one and other times favoured the
other:
·
ECG #1: circumflex OMI dominated, with subtle
LAD reperfusion
·
ECG #2: reperfusion of circumflex, LAD still
reperfused
·
ECG #3 reocclusion of circumflex and LAD
·
ECG #4-7: reperfusion of LCX and LAD, the latter
of which dominated
Take away
1.
Young people can have acute coronary occlusion.
2. Symptoms don’t always correlate with
coronary artery occlusion/reperfusion: resolved symptoms but ongoing ECG signs of occlusion
requires reperfusion.
3.
STEMI criteria is unreliable and leads to
delayed reperfusion: neither of these occlusions ever meet STEMI criteria, but
there were multiple other diagnostic signs of occlusion across the entire QRS-T
complex – including loss of R waves and new Q waves, subtle ST elevation,
reciprocal ST depression, pseudonormalization and hyperacute T waves.
4.
STEMI criteria also ignores spontaneous
reperfusion at risk for reocclusion. The question is not whether the ECG meets
STEMI criteria, but whether the patient has OMI, including reperfused OMI at
risk for reocclusion.
5.
Troponin is a delayed marker of ischemia that is
unreliable early in occlusion, or in spontaneous reperfusion at risk for reocclusion: here the first trop was only 150 and declined on
repeat, only to rise to a peak of 15,000.
6.
The angiogram can highlight occlusions at the
moment of the procedure, but it’s serial ECGs which tell the story of occlusion
and reperfusion.
7.
OMI ECG changes can be complicated by site of
occlusion, compromised collaterals to chronic total occlusions, concomitant
critical stenoses, or co-culprits – resulting in combined ECG patterns with
dynamic changes based on underlying reperfusion/reocclusion.
==================================
My Comment by KEN GRAUER, MD (2/1/2023):
==================================
Important post by Dr. McLaren, that underscores current problems with the outdated “STEMI Paradigm”. In excellent fashion — Dr. McLaren traces the evolution of ECG findings over the course of the 7 serial tracings in today’s case. Errors were made.
- Errors in today’s case resulted in a 13-hour delay. It wasn’t until the 5th ECG was obtained (apparently done only because the patient’s chest pain had returned) — that the by now markedly elevated Troponin and by now obvious ECG changes finally convinced providers of the need for cardiac cath.
- Unfortunately, significant cardiac damage had already been done. This might have been minimized had the abnormalities been picked up earlier.
Even for providers who are still “stuck” in the old STEMI paradigm — Attention to the “Take-Aways” enumerated by Dr. McLaren should help to prevent the oversights in today’s case. I focus my comment on how applying these Take-Aways at the time of the initial ECG could have prompted a much more rapid path to cardiac catheterization.
- The stuttering course of chest pain in today’s case (ie, intermittent over 2 days — and then returning ~2 hours prior to ED arrival) — is relevant for optimal management of today’s patient.
- Even clinicians still “stuck” on the STEMI paradigm need to accept that acute coronary occlusion is often a dynamic evolving process, instead of a single “static” event. The “culprit” artery acutely occludes — but then it sometimes spontaneously reopens — and, occasionally continues for a period of time to spontaneously reopen and reclose a number of times, until eventually a permanent status is reached. The stuttering course of chest pain in today’s case should have suggested this dynamic evolution — especially after seeing the initial ECG!
For clarity in Figure-1 — I’ve reproduced the initial ECG in today’s case. The tracing shows sinus rhythm — normal intervals and axis — and no chamber enlargement. There are small and narrow q waves of uncertain significance in multiple leads. (Note that rather than a Q wave — there is an rSR’ complex in lead III).
- Abnormal ST-T waves are actually present in 10/12 leads in ECG #1. While the ED physician was correct in saying that this initial ECG “did not meet STEMI criteria” — I feel there are ST-T wave changes in 3 leads that can not be ignored.
In the limb leads:
- I was not initially convinced that the subtle ST elevation in leads III and aVF was significant — until I saw the flat (“shelf-like”) ST depression in lead aVL. While not necessarily acute — given the stuttering history of chest pain over the past 1-2 days, the ST-T wave appearance in lead aVL has to be interpreted as a reciprocal change from presumed recent infarction until proven otherwise.
- In the context of lead aVL — the other high-lateral lead ( = lead I) shows a lesser degree but-still-significant amount of flat ST depression.
In the chest leads:
- There is no way that the flat (“shelf-like”) shape of ST depression in lead V2 is normal. Especially in association with an already surprisingly tall R wave in lead V2 — this (as per Dr. McLaren) is diagnostic of posterior OMI until proven otherwise. (Remember that normally — there is usually slight, upward sloping ST elevation in lead V2 — and virtually never ST depression).
- In a patient with intermittent chest pain — the straightened ST segment take-off in lead V3, with terminal T wave inversion (RED arrow) is clearly of concern. This ST-T wave appearance is not expected with posterior OMI — but instead suggests the possibility of either Wellens’ Syndrome (if chest pain has resolved) — or — reperfusion following recent LAD occlusion.
- In support of significance for the abnormal ST-T wave appearance in lead V3 — is the subtle-but-real terminal T wave inversion in neighboring leads V4 and V5.
- A final abnormal finding in the chest leads — is that the upright T wave in lead V1 is taller than the upright T wave in lead V6. Although this is a nonspecific finding — it is often associated with ischemia.
BOTTOM Line:
The history in today’s case can not be ignored. While the patient is a younger that what we usually expect to see with acute infarction — the diabetes clearly increases risk.
- While millimeter criteria for a STEMI are not met in ECG #1 — and while ST-T wave changes in most leads in the initial ECG are not definitive — the ST-T wave appearance in 3 leads ( = leads aVL — V2 — V3) can not be ignored as indication that an acute event may have recently occurred.
- At the very least — the initial ECG should have been repeated within 10-20 minutes. Seeing even subtle ST-T waves changes (such as less ST depression in lead V2, with an increase in T wave positivity in this lead — as was eventually seen when the 2nd ECG in today’s case was obtained) — would be evidence of dynamic change that confirms reperfusion from recent posterior OMI.
- The 1st troponin did come back elevated (150 ng/L). Given the worrisome history and the initial ECG — this result should have been enough to merit prompt cath.
- To Emphasize: — I had no idea from the initial ECG that there were 2 “culprit” arteries in today’s case. Had I known this — it would have explained some of the subtle contrasting ECG findings. But the point is that we do not need to know the anatomy in order to recognize that in a patient with new chest pain — the ST-T wave appearance in leads aVL, V2 and V3 of the initial ECG can not be ignored until we have actively ruled out a recent (or still ongoing) acute event.
 |
| Figure-1: I’ve labeled the 3 leads of most concern in the initial ECG from today’s case. |