On July 26, I posted a similar problem, but in that case, the huge ST elevation was proportional.
Here is another case in which it may be difficult to find the J-point if lead II was not there to help:
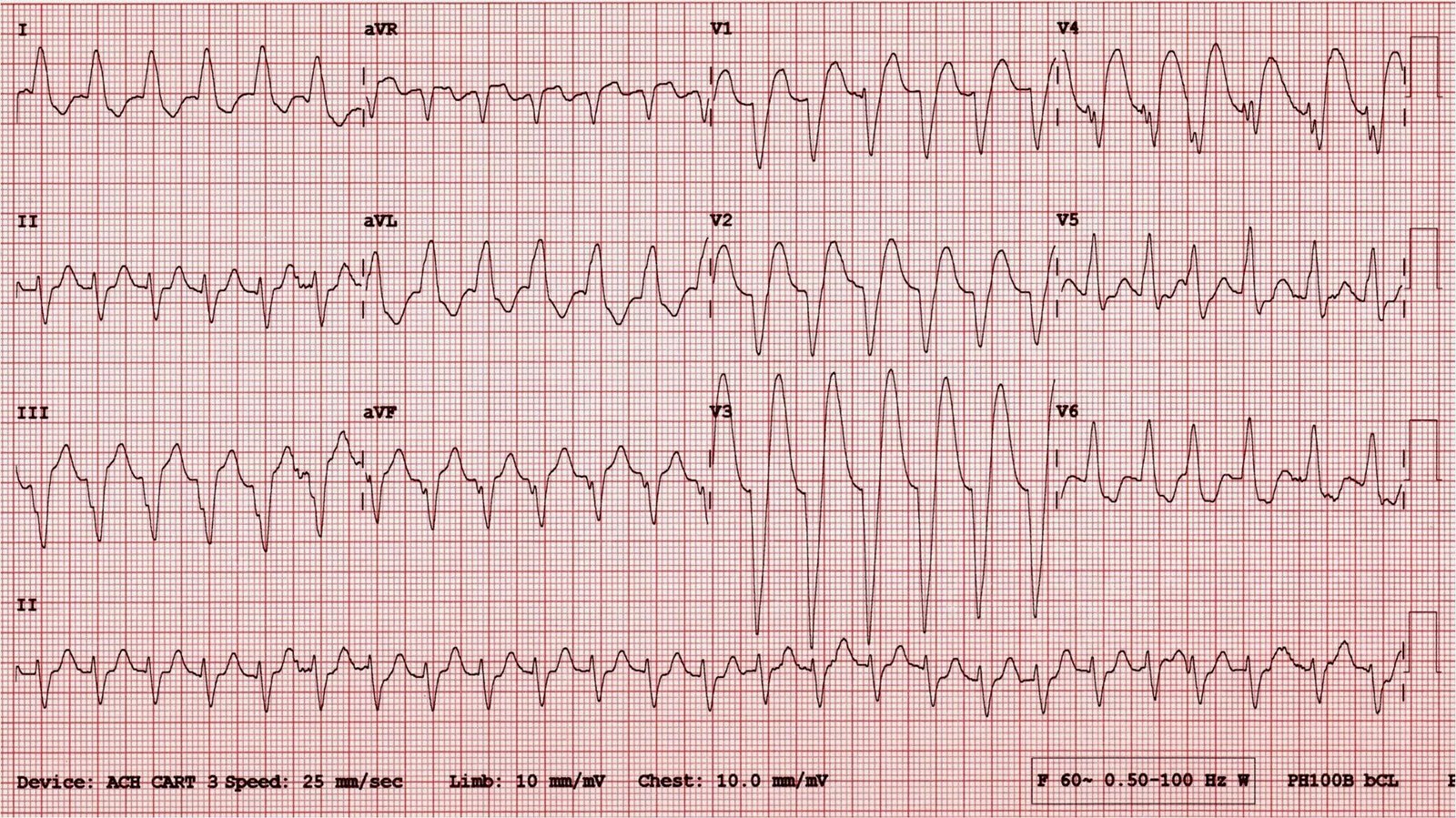
An elderly woman had a cardiac arrest, VT then PEA, and was resuscitated. Here is her initial ECG:
(In our data, a convex ST Segment in LBBB was quite specific for anterior STEMI, but only 50% sensitive)
Here is the same ECG, annotated:
 |
| Here I found the J-point in lead II and draw a line up to find the J-points in V1-V3. I have magnified this below: |
A single lead with proportionally excessively discordant ST elevation greater than 0.25 indicates STEMI
A single lead with proportionally excessively discordant ST depression greater than 0.30 indicates STEMI
However, we did not study patients with a heart rate greater than 130, as such tachycardia tends to exaggerate the ST deviation of LBBB.
Nevertheless, this is almost certainly STEMI, especially as the pretest probability (cardiac arrest) is very high.
Usually the heart rate comes down gradually after resuscitation (supportive care, diminished endogenous and exogenous epinephrine). It would be helpful to repeat the ECG after 10-15 minutes, with a slower heart rate. This was not done.
She went to the cath lab and was found to have severe 3 vessel disease, with thrombotic culprit lesions of 85% in both the LAD and circumflex. It is quite likely that these were 100% at the time of the ECG.
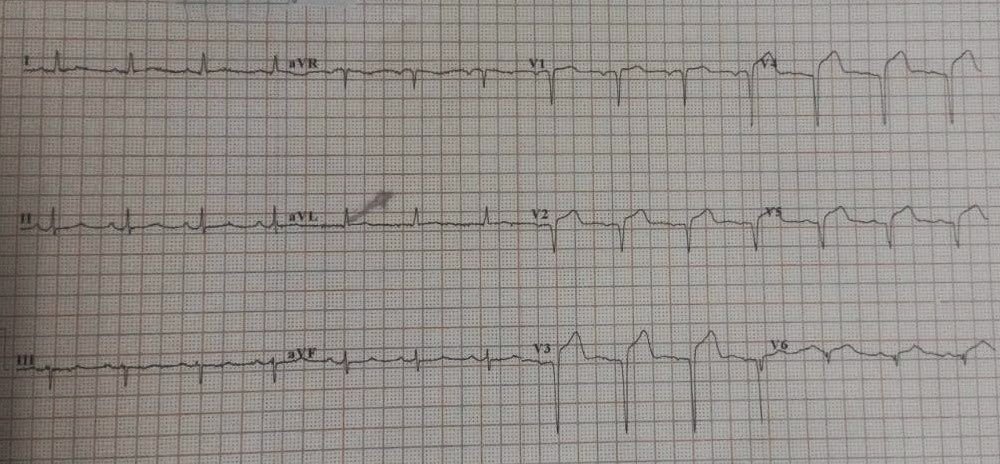
This is 3 hours after the PCI:
 |
| The left bundle branch block is resolved. There are Q-waves in anterior leads due to MI. |
The patient did well.
Lesson:
Use lead II across the bottom to help you find the end of the QRS when it is difficult to find.