A 50-something woman with PMH only significant for hypertension (treated) presented by car to the emergency department with one week of intermittent chest pain. Pt states that she had a sudden onset of central chest pain described as sharp and rated as 10/10 pain six days ago while at rest. Since then, she has been having recurrent episodes of pain lasting 2-3 minutes each time that can reach 10/10 in severity. At presentation there was only minimal chest discomfort.
She stated that she attempted taking her gastroesophageal reflux medication without relief (comment: but this begs the question: “how could that be if it only lasts 2-3 minutes?”). The pain does not worsen with movement, deep breath, or pressing on her chest. Pt also having right shoulder pain for the last two days.
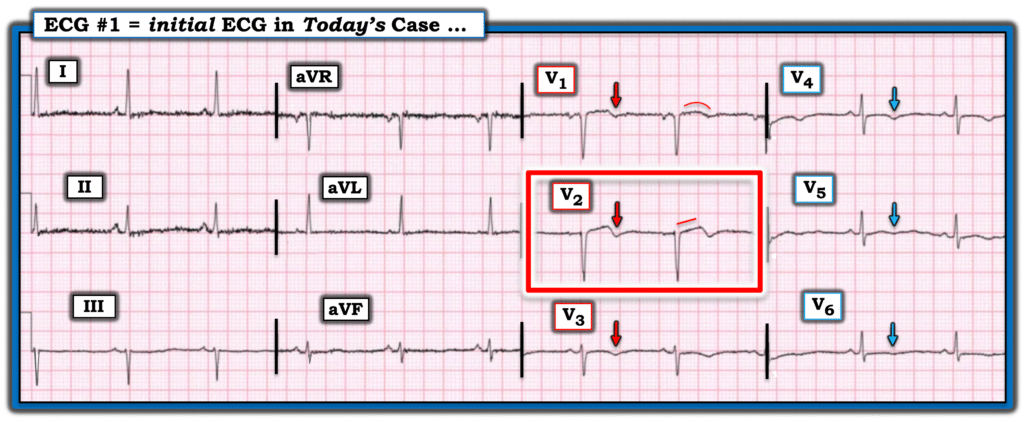
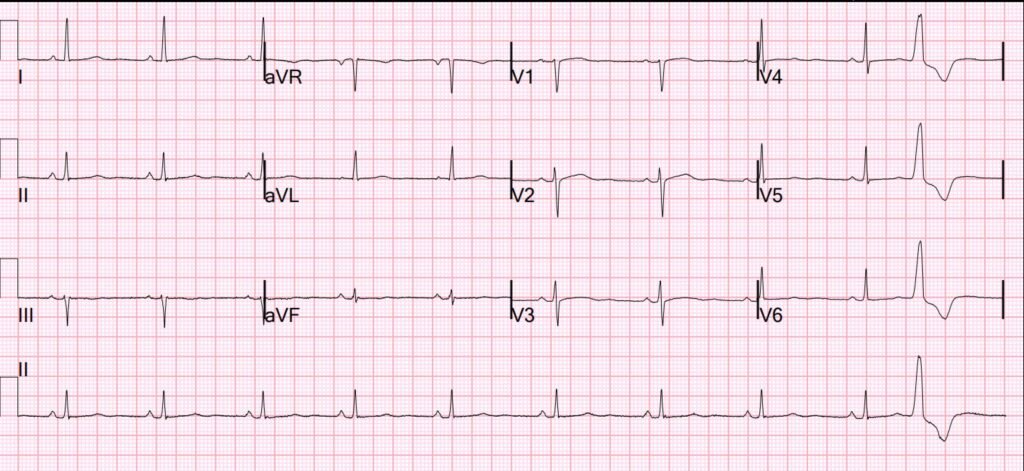
We recorded an ECG:
What do you think?
I submitted to the Queen and she asked this question:
I answered that it is Completely Resolved, and her output was “Reperfused STEMI”
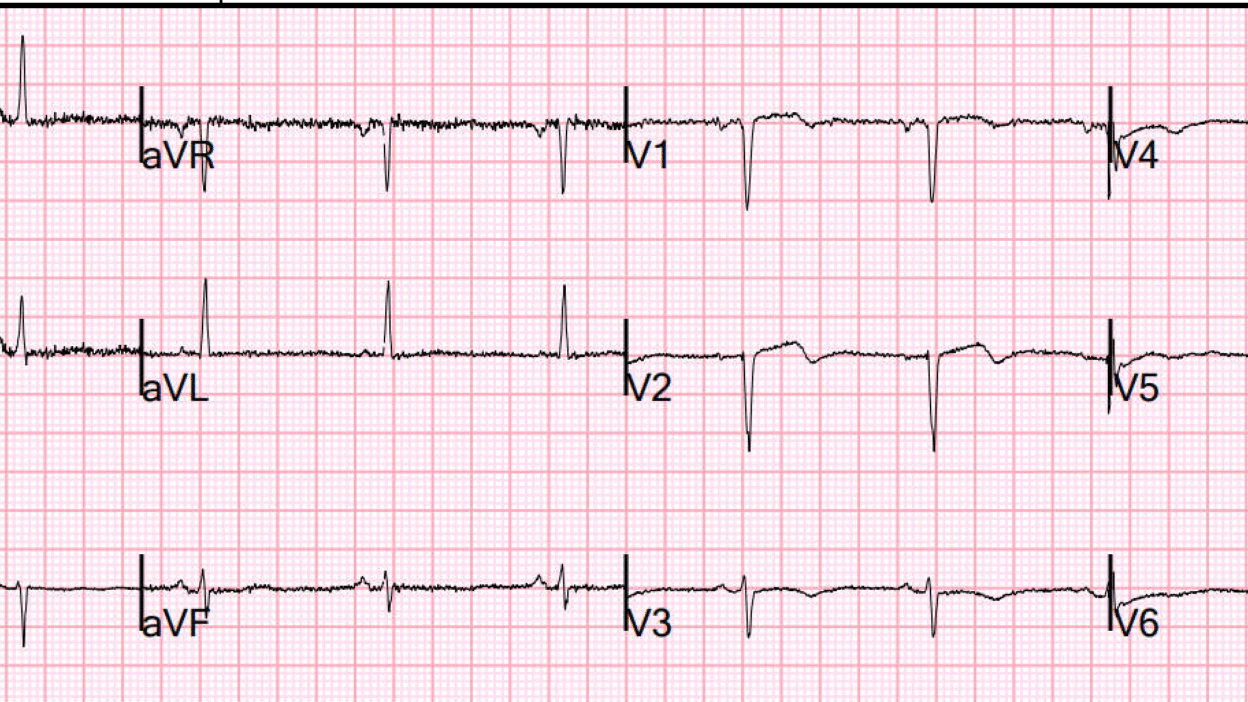
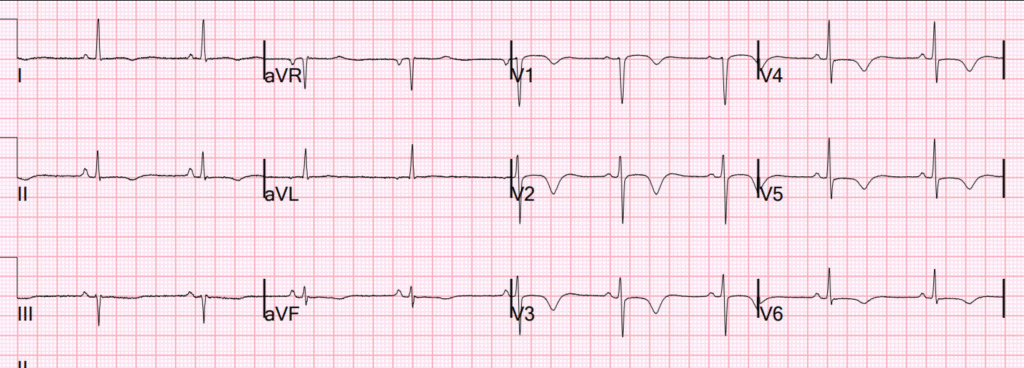
There was an old ECG available (it really is not needed however):
At first, I was afraid that this was a completed anterior infarction, with a QS-wave in V2 and shallow T-wave inversion. But then I noticed that the P-wave in V2 was inverted (it should be upright in V2) and realized the leads had been recorded too high.
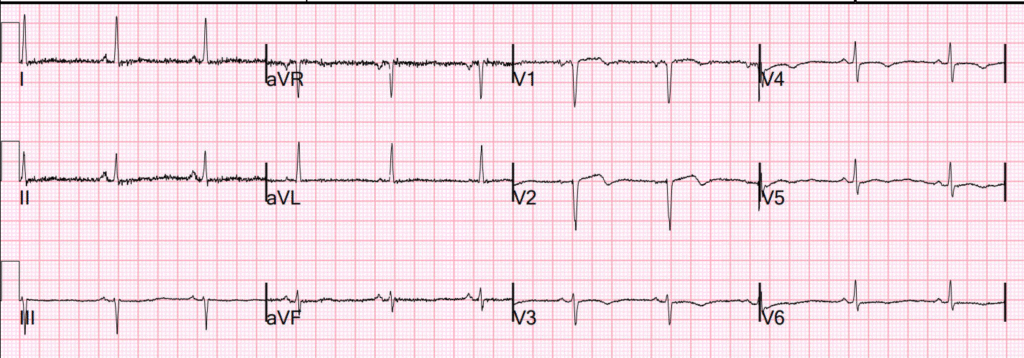
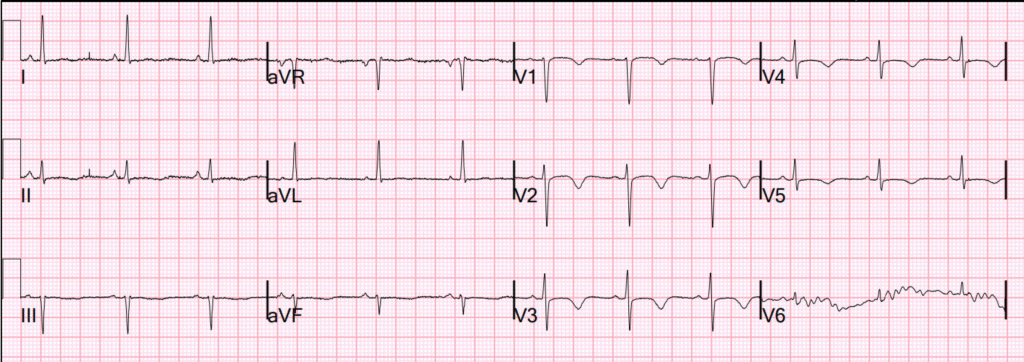
So when we recorded another ECG 1 hour later, I told the tech to put V1 and V2 lower on the chest (at the 4th intercostal space):
Now the P wave is more upright and the R-wave is now present. So complete infarction is unlikely. However, extensive T-wave inversion has now evolved, diagnostic of Wellens syndrome.
The Queen of Hearts had the same question and same answer as on the first ECG.
The patient promised us that she would report any recurrence of chest pain (Wellens is a reperfused OMI at high risk of re-occlusion; however, re-occlusion is not always associated with recurrent pain!!).
Why we need continuous 12-lead ST segment monitoring in Wellens’ syndrome.
I recorded a bedside echo and the anterior wall was normal (no wall motion abnormality)
Wellens is a transient OMI (or transient STEMI). After ST resolution in transient STEMI, we often see Wellens waves. We can often see an anterior wall motion abnormality. But one or both may be absent.
Case Continued: I was certain that this was LAD ACS. I gave aspirin and heparin, and cardiology even wanted me to add clopidogrel 300 mg to be certain she would not re-occlude before she could go to next day angiogram.
The first hs troponin I returned at 3 ng/L (almost undetectable). I was a bit surprised, but was certain that the next one would be higher.
[Abbott hs troponin I; URL for woman = 16 ng/L; Limit of Detection = 3 ng/L.]
The 2 hourtroponinreturned at 3 ng/L also!
So this was likely UNSTABLE ANGINA in the era of high sensitivity troponin (many cases here). It still happens.
The plan was not changed.
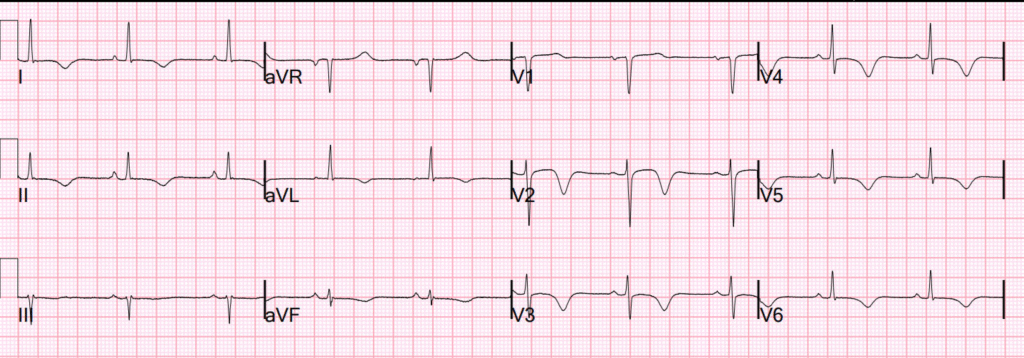
A 3rd and 4th serial ECG were recorded:
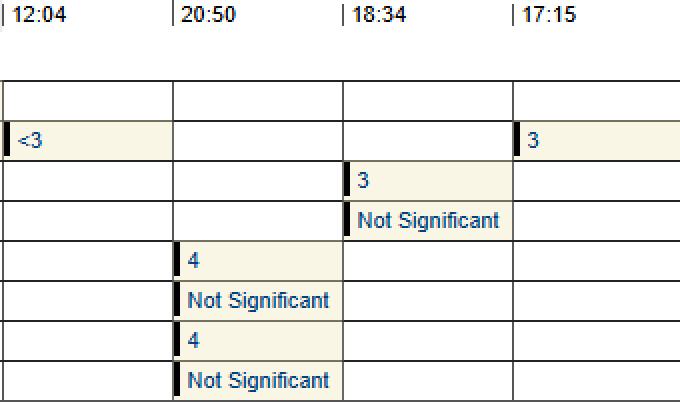
Troponin profile:
The next day, skeptical of ACS with a such a very low troponin, the cardiologists ordered a CT Coronary angiogram:
CALCIUM SCORE: The total calcium score is 45.
CT COR ANGIOGRAM: The LAD has a focal occlusion in the mid segment, with no other significant disease is present. It gives off 2 diagonal branches.
This was followed by a STANDARD ANGIOGRAM: ACS – Unstable Angina. Culprit is 99% stenosis in the mid LAD. It was stented.
Learning Points:
- All studies of troponin ruling out MI require a normal ECG!
- This is a diagnostic ECG no matter the troponin.
- Unstable Angina still exists in the era of high sensitivity troponin
= = =
======================================
MY Comment, by KEN GRAUER, MD (9/5/2025):
Today’s case by Dr. Smith is an example of expert emergency ECG interpretation at its best! Simply by reading the history — and, by seeing today’s initial ECG — I knew within seconds that this patient had a recent (if not ongoing) LAD OMI, and was in need of timely cath with PCI.
Essential Elements in Today’s History:
- The clinical setting and onset of symptoms (ie, The patient being a middle-aged woman with the risk factor of hypertension — who reports that 6 days ago she had the sudden onset of 10/10 CP). While we are not told for how long this initial CP (Chest Pain) episode lasted — it occurred at rest — and clearly was significant enough for her to remember the details of its onset.
- Since this onset of CP — the patient has continued to have CP episodes (some of which are severe) — that are not related to movement, respiration or pressing on her chest — and which are not improved by taking her reflux medication.
- Most of these recurrent CP episodes are short-lived (ie, lasting only 2-3 minutes).
- There has been radiation of her CP, such that she has had unexplained shoulder pain for the past 2 days.
- While not completely gone, her CP at the time that the ECG in Figure-1 was recorded — is now much less than it had been during the previous 6 days. That said — her experience over these past 6 days was worrisome enough to her that she presented by car to the ED for evaluation.
= = =
My Interpretation of Today’s History:
Today’s patient clearly describes a worrisome history that is potentially consistent with an acute cardiac event (ie, especially that her symptoms were not alleviated by any of the self-help measures she tried).
- The fact that her onset of symptoms began 6 days earlier, and have persisted, although being less severe at the time ECG #1 was recorded — tells us that there may have been some element of spontaneous reperfusion — and, that any ECG changes we might see could be subtle (ie, If ECG #1 was recorded during the process of “pseudo-normalization” ).
- Finally — The fact that this patient’s most severe CP episode occurred 6 days earlier, and recurrent episodes have been of brief duration — tells us that the initial 1 or 2 Troponin values might be no more than minimally (if at all) elevated.
= = =
Today’s Initial ECG:
All of the ECG findings in Figure-1 are explained by the above history:
- My “eye” was immediately drawn to the ST-T wave in lead V2 (within the RED rectangle in Figure-1). The ST segment in this lead is straightened, and although there is no significant ST elevation — we see the biphasic T wave (initially positive — with terminal T wave negativity) that is so typical of Wellens’ Syndrome.
- To Emphasize: Today’s case does not satisfy the strict definition of “Wellens’ Syndrome” — because although this patient’s CP has improved since it began 6 days earlier, it has not totally resolved (as it should with true Wellens’ Syndrome). That said, given improvement in this patient’s CP and the characteristic ECG picture in lead V2 — I suspected similar clinical implications of Wellens’ Syndrome.
- Consistent with recent (and/or ongoing) LAD OMI — is subtle-but-real ST segment coving with terminal T wave inversion in neighboring leads V1 and V3. Subtle T wave inversion persists in leads V4,V5,V6 (BLUE arrows in these leads).
- ST-T waves are remarkably flat in the limb leads. While this is a non-diagnostic ST-T wave change — it is definitely not “normal” — and consistent with the overall clinical picture.
BOTTOM Line: While additional evaluation as described above by Dr. Smith was clearly essential (ie, repeat ECG with correction of V1,V2 lead placement — comparison with a prior tracing on this patient, serial Troponins) — I knew within seconds of learning the history and seeing the initial ECG what timely cardiac cath would show.
- Although somewhat surprising that serial Troponins were unremarkable — the onset of symptoms 6 days earlier, and the very brief duration of repeat episodes should have prepared the cardiology team for this possibility.
- The ECG picture in Figure-1 serves as an important reminder of the importance of correlating the patient’s history — with the initial ECG.
= = =
Figure-1: I’ve reproduced and labeled today’s initial ECG.