This was sent by Kirk Lufkin and was diagnosed by a Physician Assistant who works with him by the name of Danielle Hutcheson. They work in a remote hospital without PCI capability. Kirk and I graduated from residency together in 1990, and he has taken up the OMI paradigm with enthusiasm. He showed Danielle the blog and she has started reading it regularly.
Case
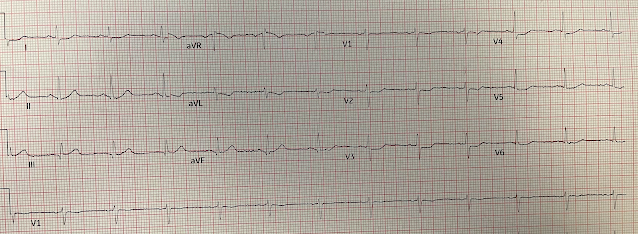
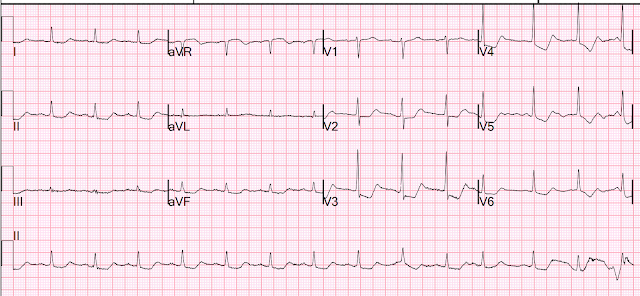
A 50-something male with HTN, past smoker, no h/o CAD presented with chest pain. Here is the first Emergency Dept EKG:
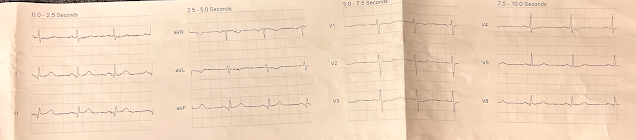
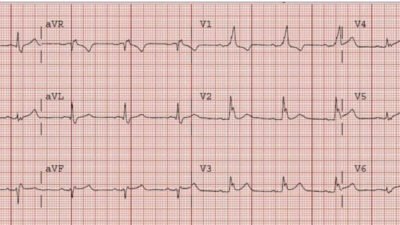
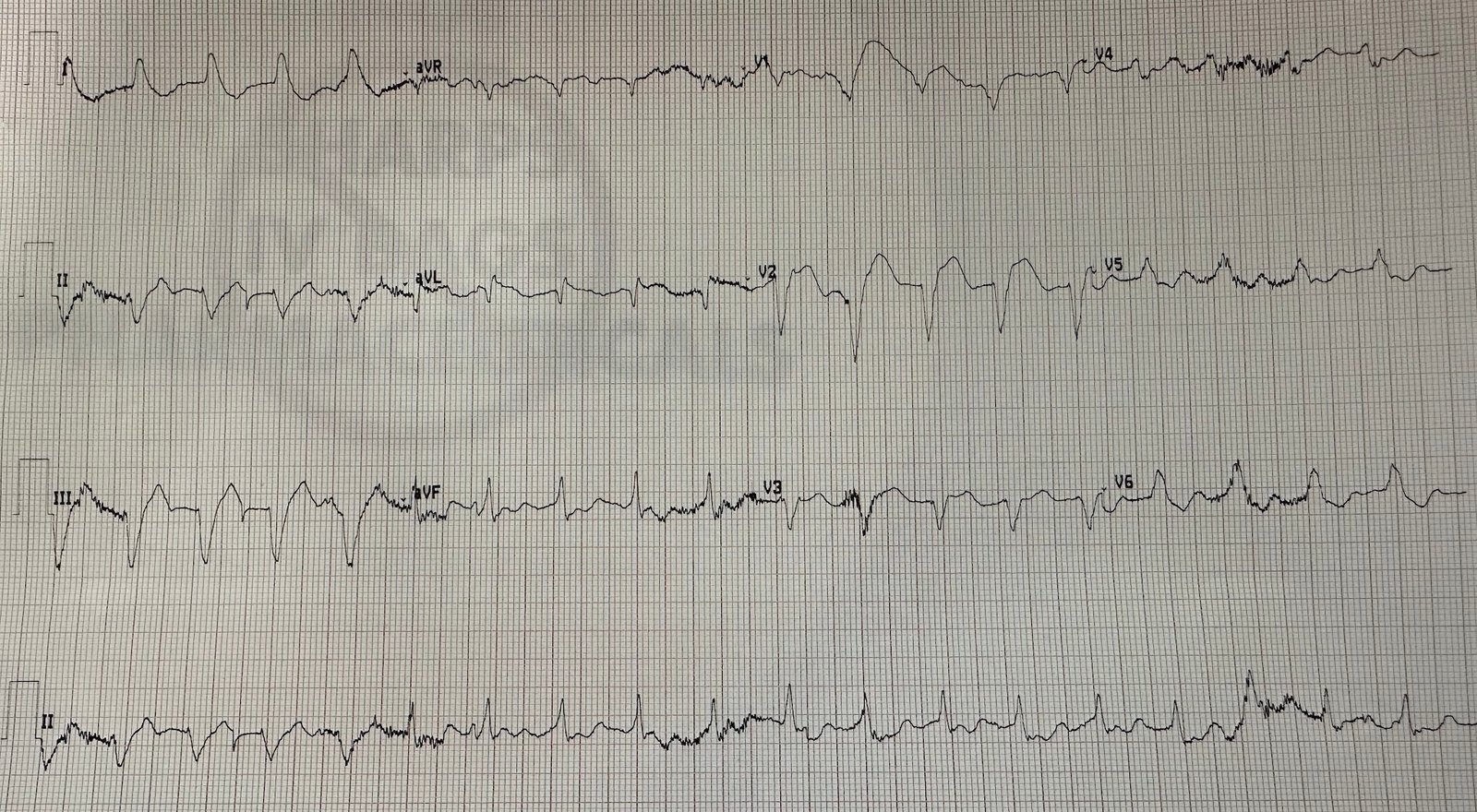
Note the subtle hyperacute T-waves in inferior leads (inferior OMI), the negative T-wave in V2 which confirm additional posterior OMI, and the absence of STE in posterior leads V7-V9. This was a proven inferior posterior OMI.
Learning Points:
1. You should be more certain of OMI diagnosis when giving thrombolytics because they are more dangerous than PCI. Even in low risk patients, the risk of intracranial hemorrhage is nearing 2%. But if the clinical and ECG diagnosis is certain, there need not be ST Elevation meeting millimeter criteria. This means that you must be expert at the diagnosis, or use the Queen of Hearts.
2. Posterior leads frequently have false negatives. If the standard 12-lead is diagnostic, do not let absence of posterior ST Elevation dissuade you.