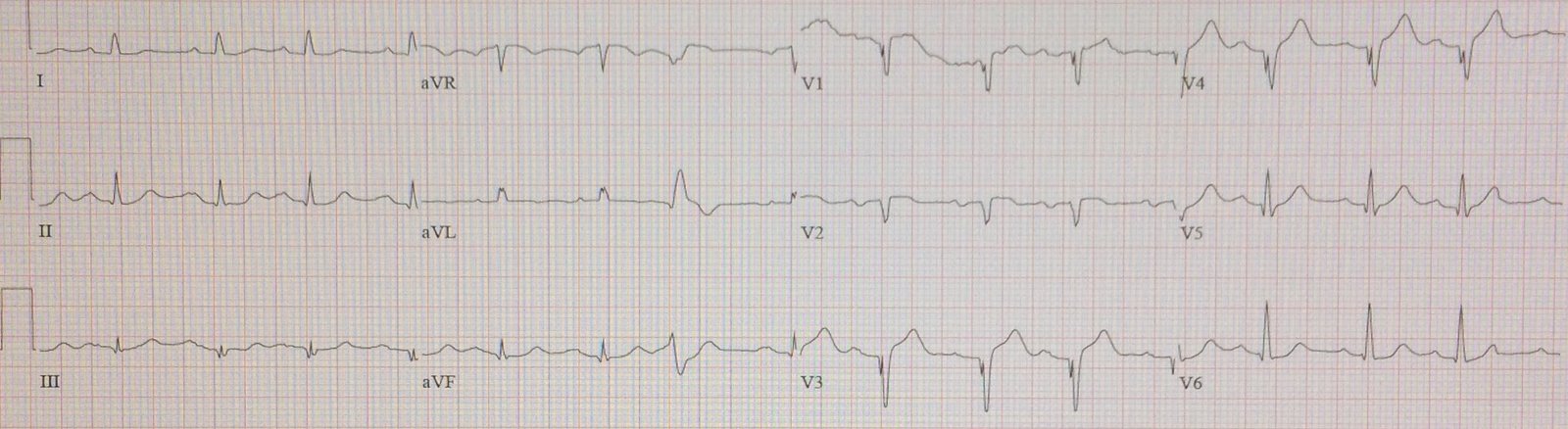
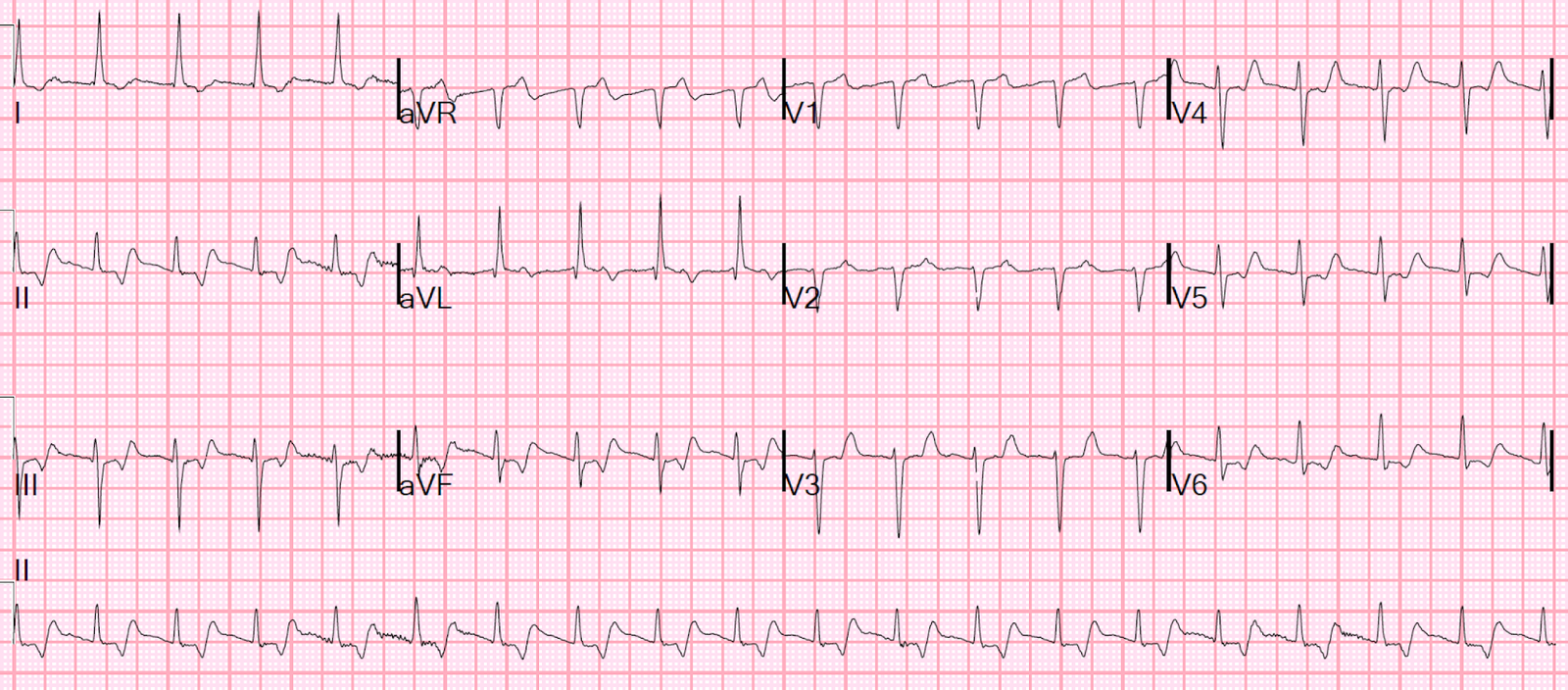
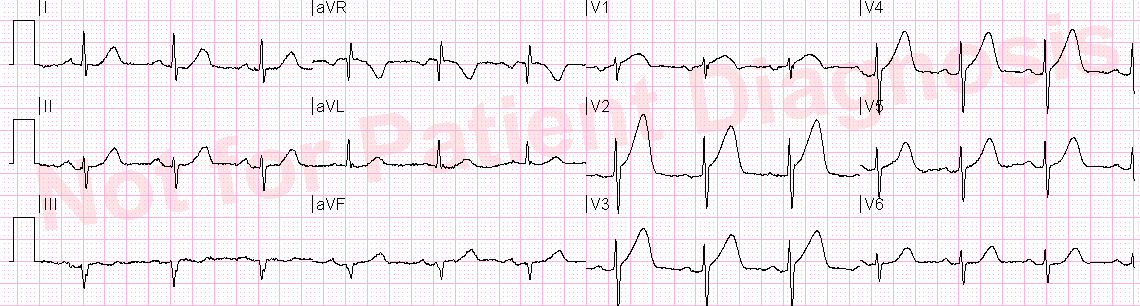
This ECG was sent along with this text:
“Thoughts? Occlusion or not? – context : cardiac arrest:”
Aside: Ryan Tee also noted correctly that there is also a PVC in aVL with concordant ST elevation. This is a very good sign for STEMI, but it could possibly also be seen in LV aneurysm.
Comment
One might say that any shockable cardiac arrest should go to the cath lab emergently, and there are many good arguments for that. Most of these arguments are based on “if there is no alternative explanation.”
Old MI is such an alternative explanation, as it supplies the underlying substrate (scarred myocardium) that leads to ventricular fibrillation.
Furthermore, not all hospitals actually take all shockable cardiac arrests for angiogram, but rather do so selectively for those with ECG evidence of ischemia (especially, of course, STEMI).
In this case there is a clear alternative diagnosis: old MI, and no obvious ischemia on the ECG.
But that is only true if you do not understand the T-wave in old MI: it is not large, but rather small or slightly inverted.
The T-waves were too large and upright in V3 and V4 to be due to old MI. They had to be acute (or, I should say, subacute). This is confirmed by the initial troponin of 11, which is only present in MI that has been going on for “a while” (at least 6 hours).
Brooks Walsh recently wrote this post which explains it all in much more detail.


You could distinguish new vs old regional wall abnormality by wall thickness? Is initial troponin. However a result of CPR followed by electrical cardioversion?
What about fragmented QRS in leads (V1, V3 ,V4) which represent scarred myocardium due to previous MI that cause fatal arrhythmia ?
Mostafa,
I did not mention that, but good point. It could also be due to subacute MI, not necessarily old MI.
Steve
Dave,
Yes, You could distinguish old vs. new.
But you could not distinguish old vs. old with superimposed new. Only the T-wave does that.
A troponin of 11 is too high for CPR/cardioversion. Those are < 3
Steve
Great post, Steve! And the link to the other Walsh article is excellent as well. There are a few other interesting findings on the ECG (though certainly none would not have usurped the urgency of determining the need to go to the cath lab immediately).
Did you notice the width of some of the P waves? Very wide. There is also an atrial bigeminy throughout the tracing. The P waves in V1 are not easily seen (except for one) but the negative component in V2 appears to show some prominence. I think this most likely represents a left atrial abnormality due to atrial enlargement or an interatrial block (there's also a 1st degree AV block). Do you know if anything was ever revealed about the patient indicating why there would be an LA abnormality or if there was any other evidence of LVH?
Jerry,
Good observations, but I know nothing else about the patient.
Thanks!
Steve
An impressive case. This patient may had old MI with LV aneurysm and the typical V5-6 T wave should be discordant to QRS? But this EKG is concordant. Did this also be a hint of subacute STEMI?
Discordance and concordance do not apply to LV aneurysm. As stated in the post, from the ECG alone it could be aneurysm + superimposed acute STEMI, or subacute STEMI.
can you talk a little bit more about the concordant ST elevation in the PVC's. how much can you read into the morphology of the PVC? Thanks!
There are no formal studies of this, but in my experience, you can treat PVCs ALMOST like bundle branch blocks. concordant ST elevation or depression, or excessively discordant (by proportion > 25%) ST elevation or depression is all but diagnostic of transmural ischemia.
Steve Smith
thanks!