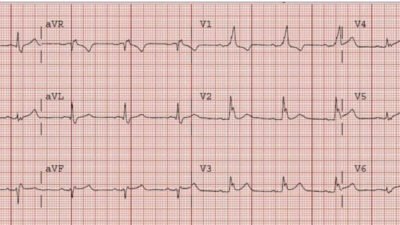
This elderly patient had an accidental carbon monoxide poisoning. The patient did not have ischemic symptoms, but we do an ECG routinely to look for ischemia. Here it is:
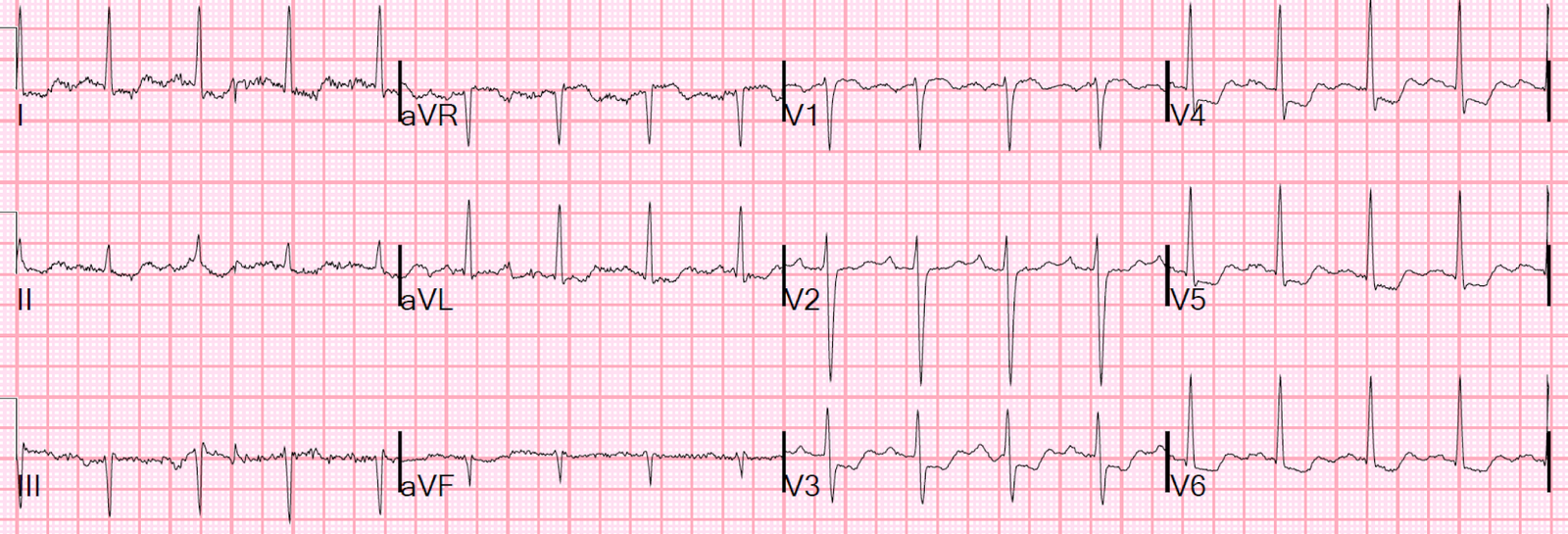 |
| There is ischemic ST depression, typical of diffuse subendocardial ischemia. |
The CO level returned at 28%.
Carbon Monoxide displaces oxygen from hemoglobin, and thus effectively decreases oxygen saturation, in this case by 28%, down to 72%. But it also binds with cytochrome oxydase to inhibit ATP formation. Thus, its effect is the same as ischemia.
We consider cardiac ischemia (on the ECG, or by elevated troponin), by itself, to be an indication for emergent hyperbaric oxygen (HBO) even if there are no other indications such as neurologic disability, loss of consciousness, level greater than 40%, pregnancy, or other indications.
We happen to haveone of the world’s finest hyperbaric oxygen facilities here at Hennepin County Medical Center (HCMC). Dr. Cher Adkinson designed and built the center, and it is now run by our director of Hyperbaric Therapy, Chris Logue, MD.
We treat many chronic conditions with , but are open 24/7/365 for emergencies including CO poisoning, air embolism, decompression sickness, and central retinal artery occlusion.
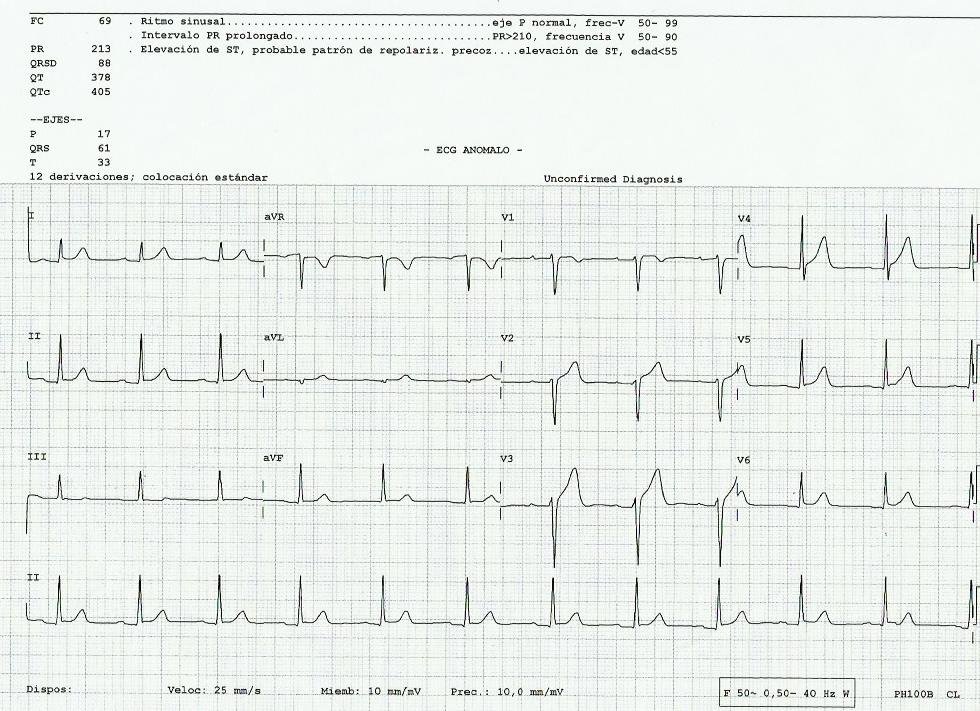
The patient underwent hyperbaric oxygen therapy. Here is her ECG afterwards:
 |
| There is only minimal residual ST depression. |
The troponin I peaked at 5.1 ng/mL.
Dr. Adkinson’s research here at HCMC, published in JAMA, found that myocardial injury (as indicated by troponin elevation, but also by ischemia on the ECG) is common in carbon monoxide poisoning and is independently associated with an increased risk of mortality at 7-year followup (38% vs. 15%). A subsequent publication in JACC reported that myocardial injury was not at all predicted by CO level.
Echo after HBO showed:
Normal estimated left ventricular ejection fraction – 65%.
No wall motion abnormality
Normal left ventricular size.
The patient did well.