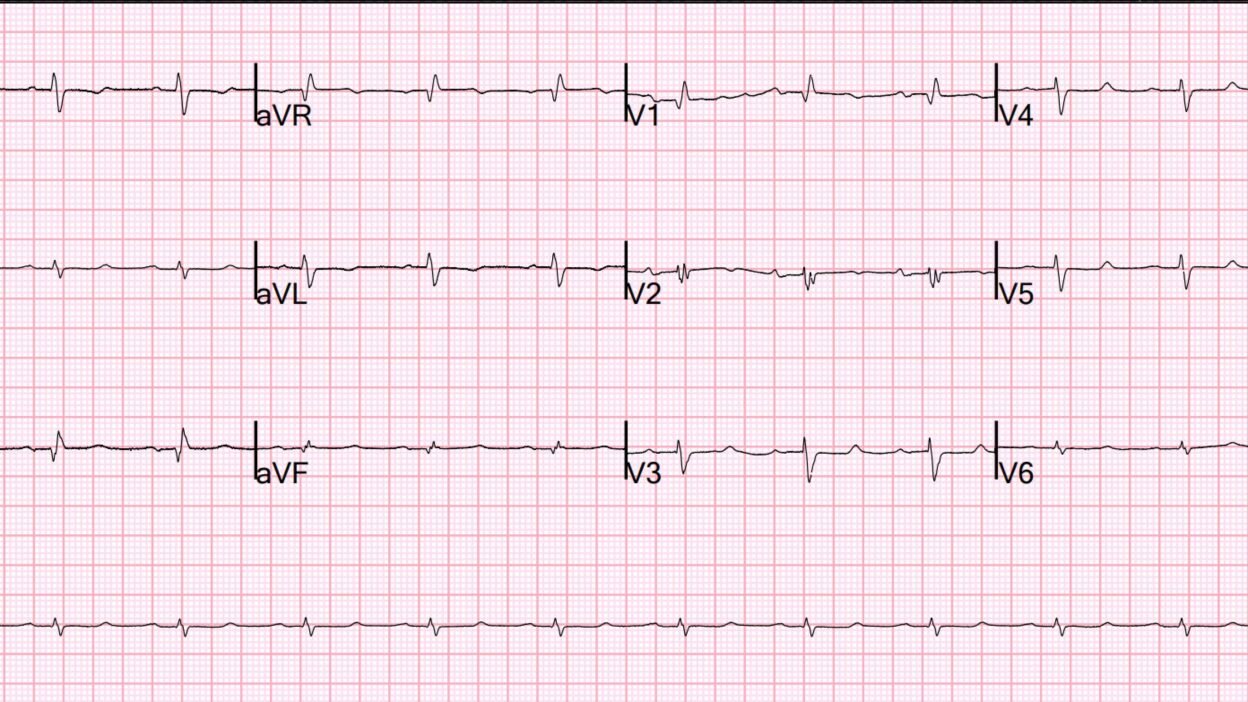
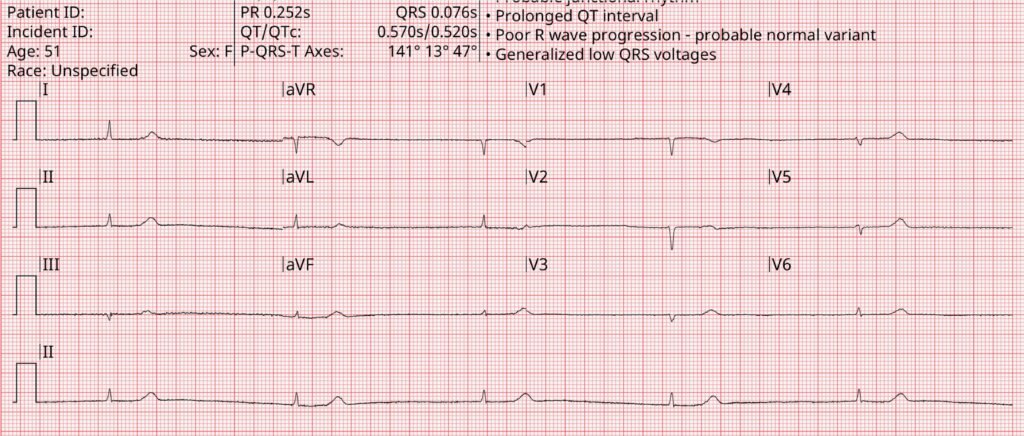
ECG 1:
What do you think? Then you can look at the rest.
ECG 1: This is hyperkalemia. As soon as I saw it, I knew it. The peaked T-waves of hyperK are not always tall a peaked. Sometimes they are just small triangles, as in this case. T-waves like this are not seen in anything else. To me, they are almost pathognomonic. Lab results: K = 6.3; ionized Calcium = 4.0 (slightly low, explains long ST segment — typical of dialysis patients)
Extra credit: There is also right axis deviation and a large R-wave (R/S > 1) in V1, so this is Right Ventricular Hypertrophy (RVH) also.
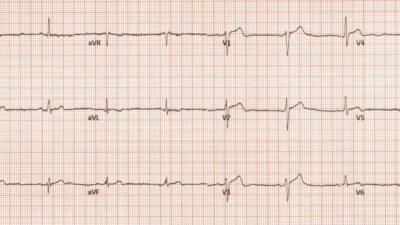
ECG 2:
ECG 2: HyperK immediately recognized by Smith. Stat placed. K = 6.2
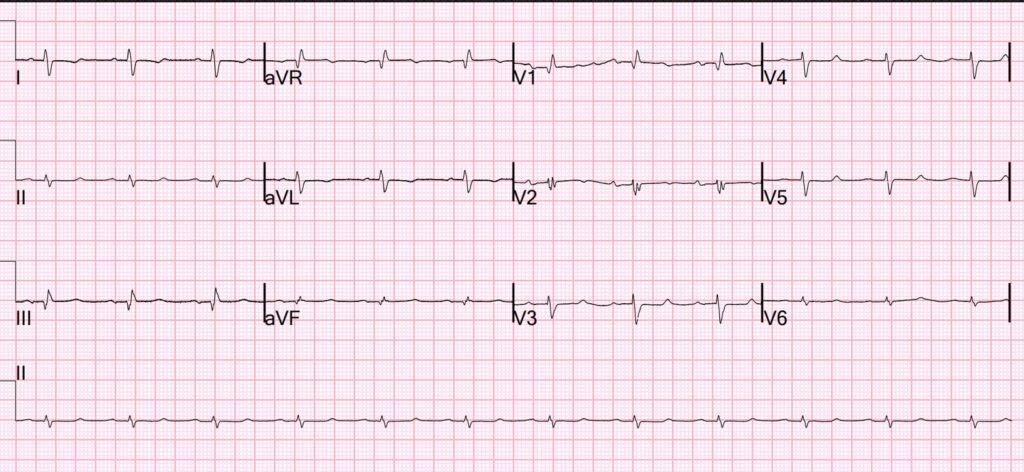
ECG 3:

ECG 3: hyperkalemia 7.1. Pseudo-OMI. Cath lab activated falsely.
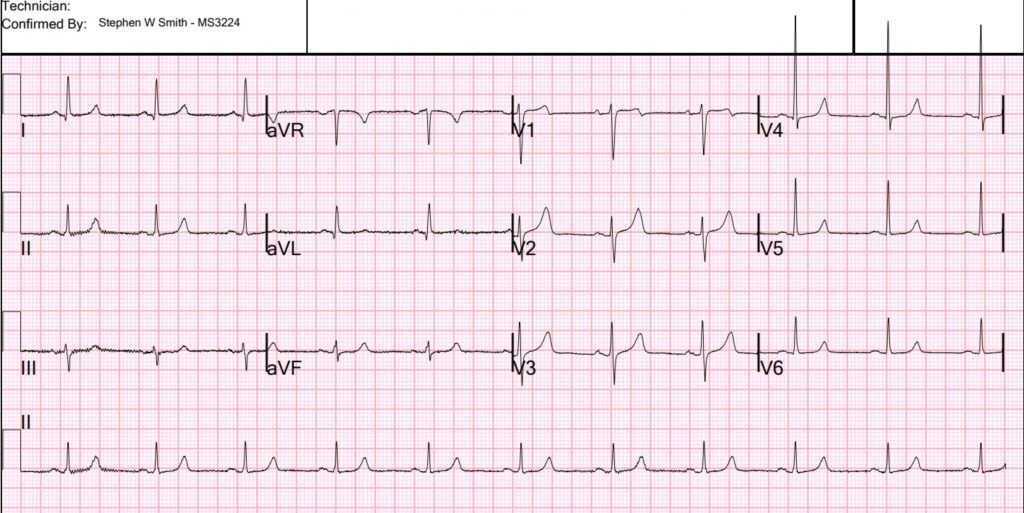
ECG 4:

ECG 4: K = 6.3. Called “normal”. Patient arrested.
ECG 5:
ECG 5: K = 7.1. This one is easy due to bradycardia. But still look how small the T-waves are.
ECG 6 (below): K = 6.8. See this full case here from this post, with lots of other fascinating HyperK cases!!
Learning point:
Hyperkalemia T-waves are not necessarily tall and peaked; they may be very short and peaked, like a small triangle. I have learned to recognized these instantly and accurately.
= = =
======================================
MY Comment, by KEN GRAUER, MD (12/21/2025):
The diagnosis of hyperkalemia is easy — when the QRS is wide with tall, peaked T waves on ECG and the clinical situation is obvious (ie, renal failure, acidosis, ingestion of K+ retaining medications). The diagnosis is far more elusive when the QRS is not wide and T waves are not tall and peaked.
- The reality is that failure to promptly identify and treat severe hyperkalemia is a potentially lethal oversight. Yet the multifaceted “ECG identities” of hyperkalemia make recognition of its more subtle presentations an ongoing challenge.
= = =
Subtle “ECG Identities” of Hyperkalemia:
- Unlike the dogma that used to be taught (ie, That there is a set “sequence” of ECG changes that are seen with progressively increasing degrees of hyperkalemia) — many patients “do not read the textbook”. Thus, the clinical reality is that any combination of ECG changes can be seen with virtually any elevated level of serum K+. In the extreme — this includes the possibility of cardiac arrest as the 1st manifestation of hyperkalemia (without QRS widening, loss of P wave amplitude; various bradyarrhythmias and AV blocks — and even without any T wave peaking! — See My Comment in the August 22, 2025 post).
- Among cases of Brugada Phenocopy published on Dr. Smith’s ECG Blog (in which a Brugada-1 ECG pattern is precipitated by some underlying condition) — hyperkalemia is the most common cause. As with other causes of Brugada Phenocopy — this ECG sign usually disappears promptly once hyperkalemia is treated (See My Comment in the May 5, 2022 post — and the January 13, 2025 post). Therefore — I always consider the possibility of hyperkalemia whenever I see an unexpected Brugada-1 ECG pattern in which there is QRS widening.
- Rhythm assessment may be especially challenging with hyperkalemia because: i) The QRS may widen, often with an unusual QRS morphology that suggests a ventricular rhythm; — ii) P wave amplitude may decrease (and P waves may even disappear = sinoventricular rhythm); — iii) Bradyarrhythmias are common — often with 1st-degree AV block and/or with other forms of AV block that often “do not obey the usual rules” for rhythm interpretation; — and, iv) Ultimately VT may develop, but — Is the regular wide rhythm without P waves VT? — or perhaps a sinus or junctional rhythm with loss of P waves due to hyperkalemia? (See My Comment in the January 16, 2022 post).
- Significant hyperkalemia is notorious for masking ECG signs of ischemia/infarction (See My Comment in the September 5, 2022 post). This is because the ECG shows us the net effect of hyperkalemia and whatever other condition(s) may be operative. For example — IF T waves were peaked because of hyperkalemia — What will happen to such T wave peaking if acute ischemia on the baseline ECG was causing ST depression/T wave inversion?
- And then there is the patient who presents with marked QRS widening and a potentially lethal elevated serum K+ level — who is surprisingly alert with normal vital signs despite a QRS duration approaching 1 large box in duration (See My Comment in the July 14, 2025 post).
= = =
Hyperkalemia with Small T Waves:
In addition to the above subtle ECG “identities” of hyperkalemia, is the “theme” of today’s discussion by Dr. Smith — which in essence, is that the T waves of hyperkalemia are sometimes surprisingly small.
- KEY Point: If you see multiple symmetrically peaked T waves (even if small) — then consider hyperkalemia (especially if the clinical situation is potentially consistent for association with hyperK).
= = =
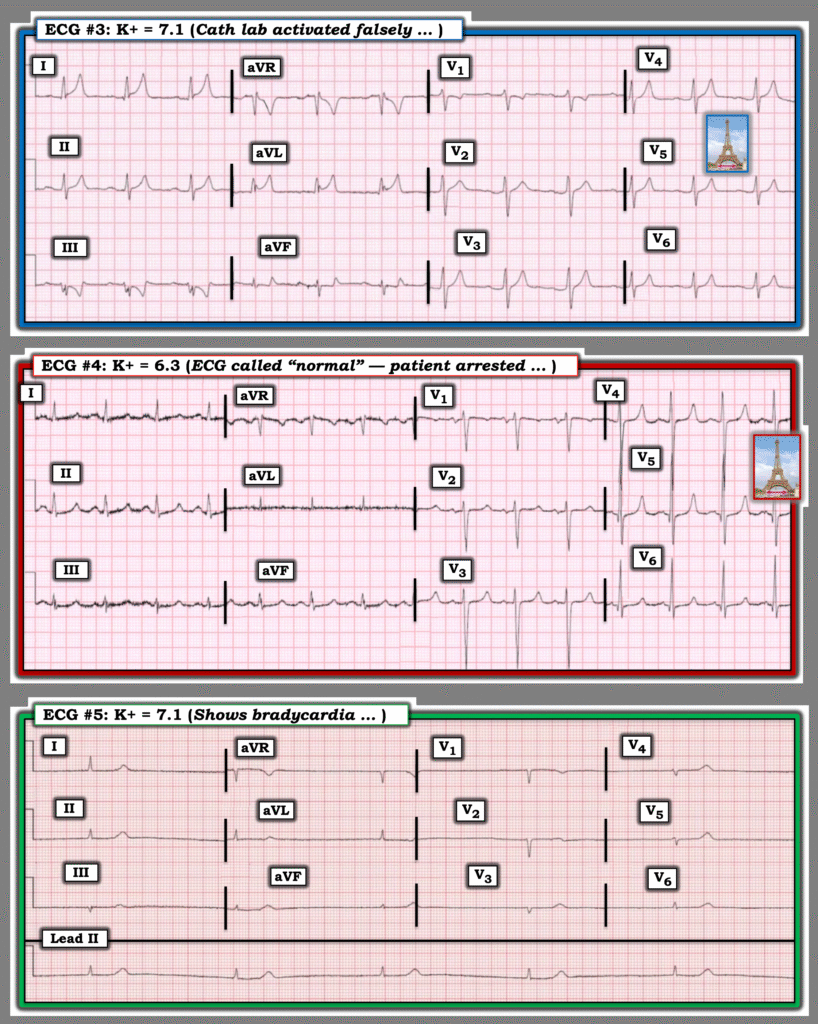
For clarity in Figure-1 — I’ve reproduced 3 of the tracings from Dr. Smith’s discussion that I’ll briefly comment on:
= = =
Figure-1: ECGs #3,4,5 from Dr. Smith’s above discussion.
- ECG #3: The T wave peaking in this tracing fooled providers into thinking these were the hyperacute T waves of an acute OMI. Clues to hyperkalemia include: i) Diffuseness of this T wave peaking (in no less than 8/12 leads); — ii) Shape of these T waves (very pointed at their peak); — and, iii) Awareness that the T waves of hyperkalemia are not always positive — but the T wave peaking may be negative (as it is here in lead III ).
- ECG #4: The T waves in leads V3,V4 manifest the typical “Eiffel Tower” effect of hyperkalemia ( = symmetric T wave shape, pointed at their peak, with a narrow T wave base). While T waves are relatively small in other leads — the small, symmetric triangles described by Dr. Smith are clearly present in most other leads.
- ECG #5: The QRS is small and narrow — and tall, peaked T waves are not seen. But: i) The rate is very slow; — ii) P waves are absent (? sinoventricular rhythm?); — and, iii) Even though small and not particularly pointed — T waves are disproportionately tall considering how tiny the QRS is — and these T waves do form symmetric triangles. We need to condition ourselves to consider hyperkalemia with this type of tracing.
= = =
= = =