Sent by anonymous
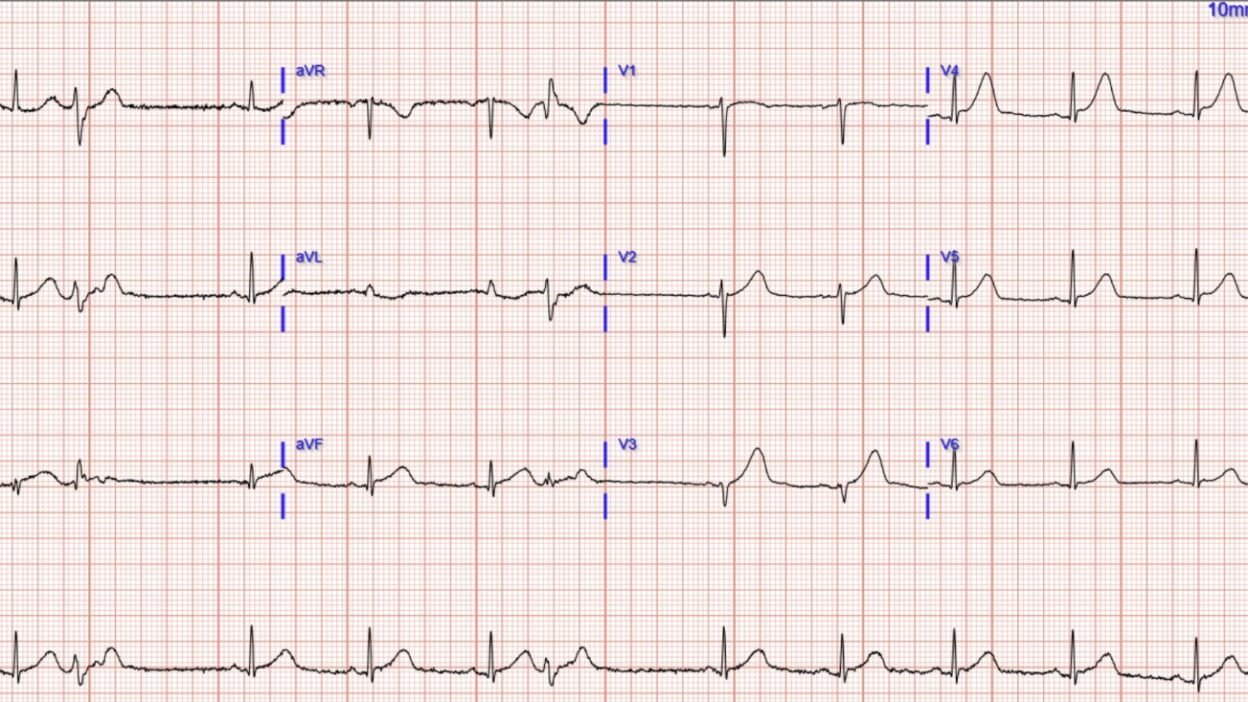
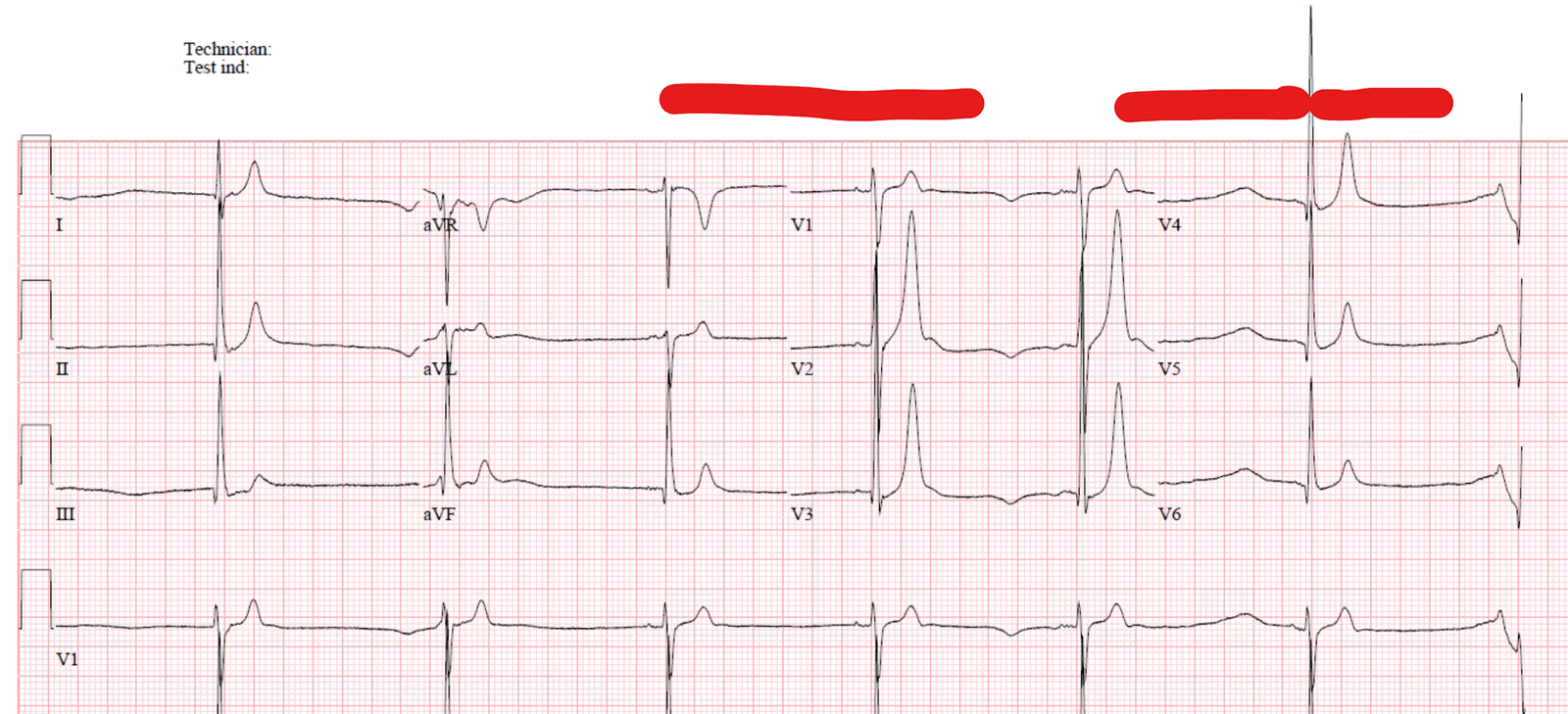
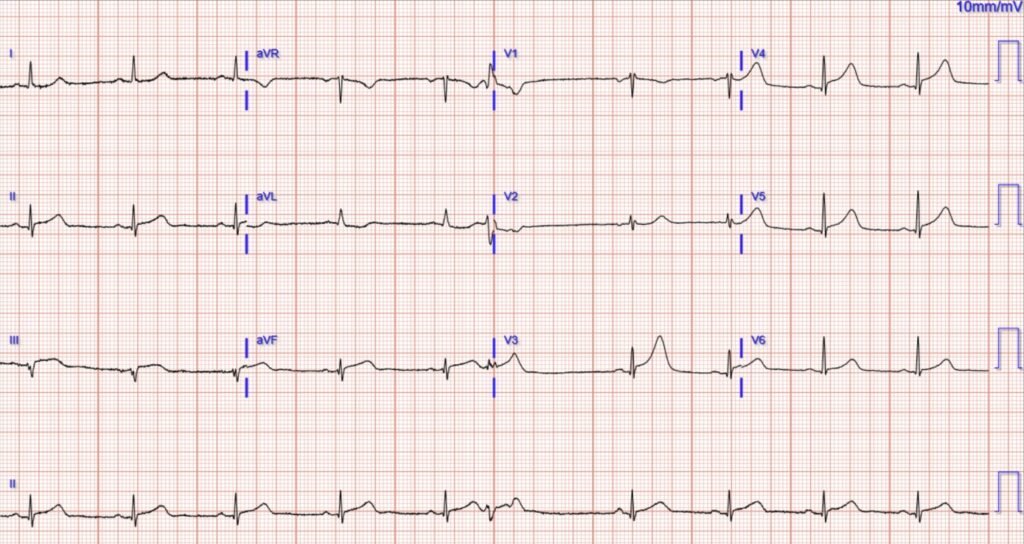
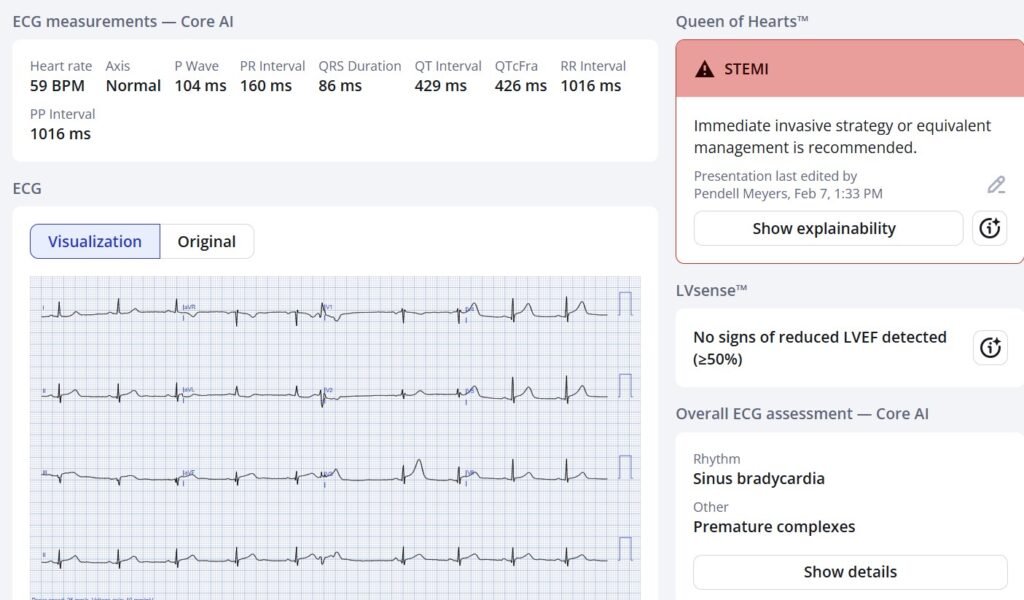
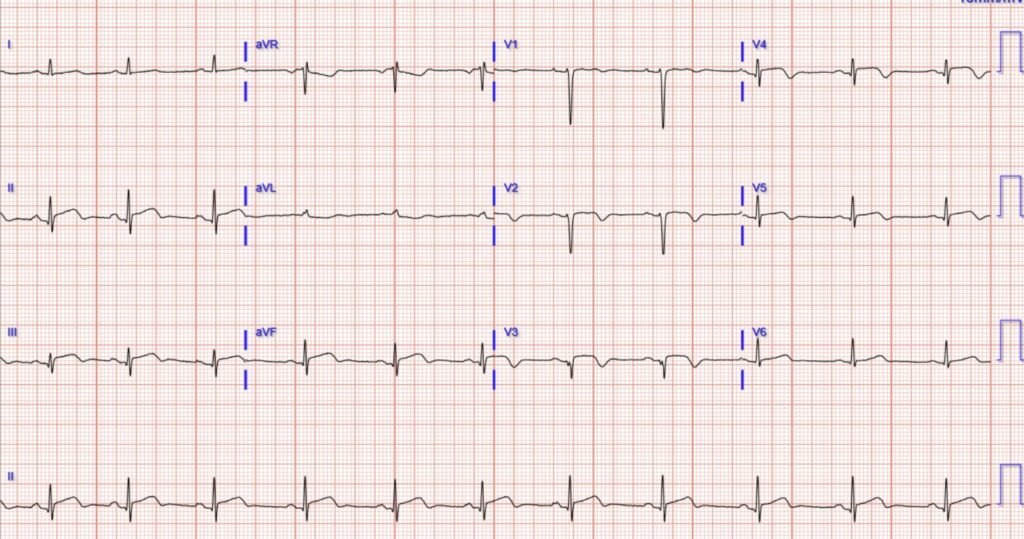
A woman in her 40s presented with acute chest pain. Her vitals were within normal limits. Here is her triage ECG:
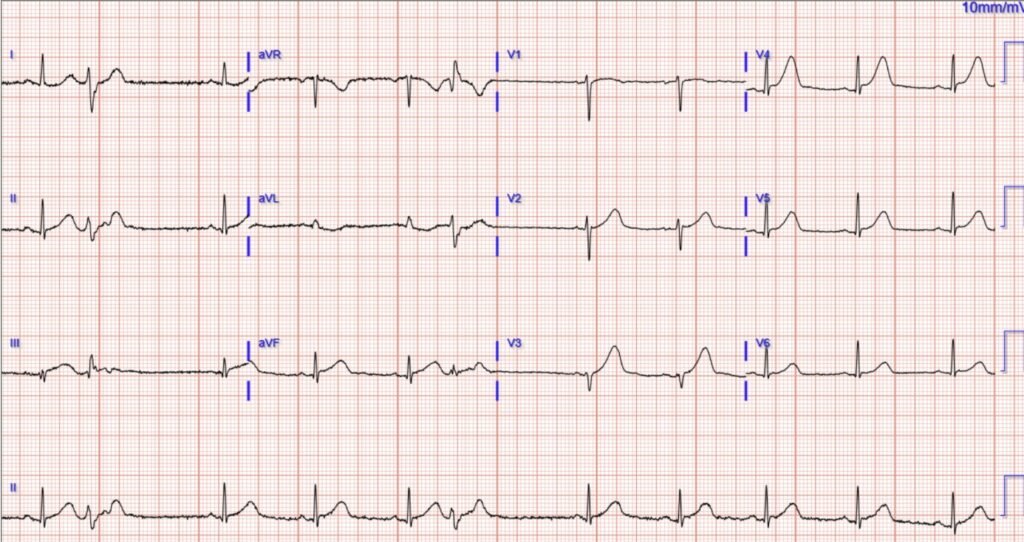
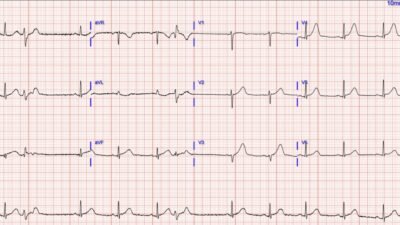
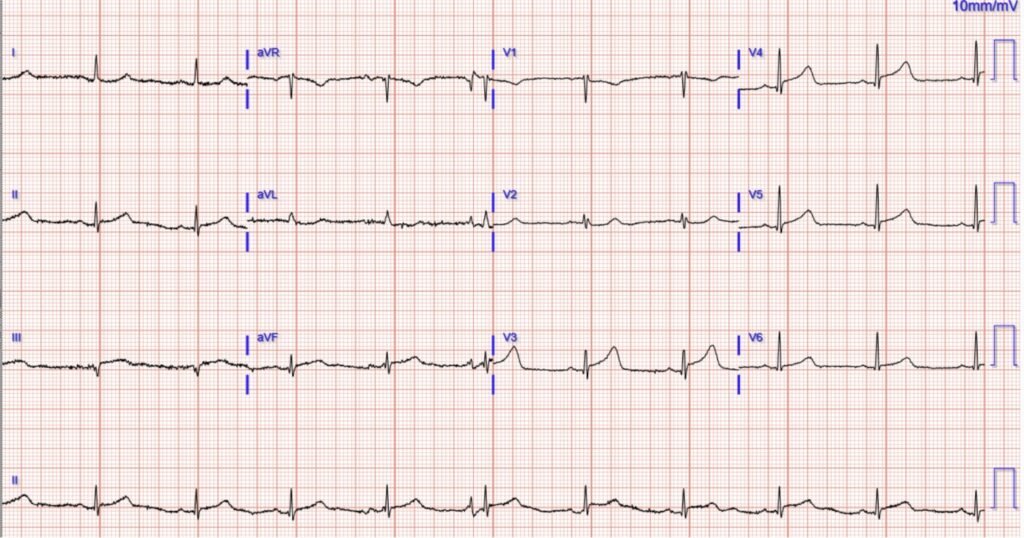
Readers of the blog will not need any baseline ECG for comparison. But here it is for those who need it:
What do you think? Will this patient actually get timely care at your facility?
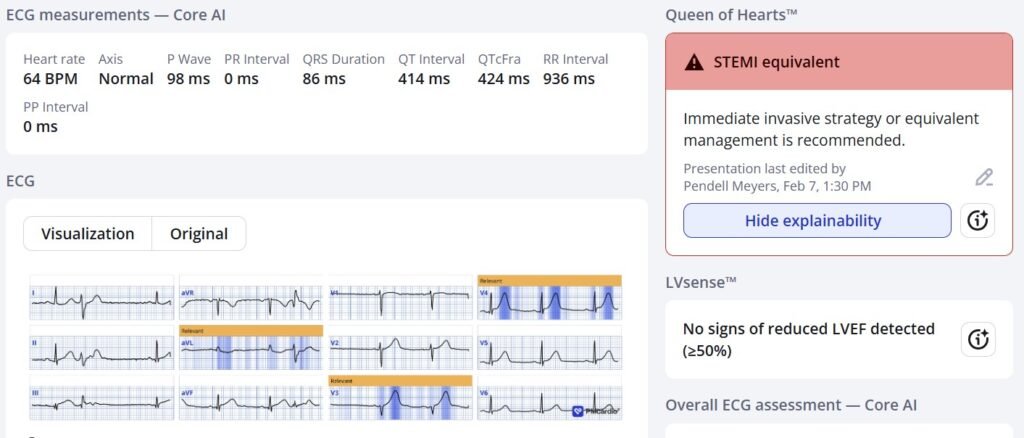
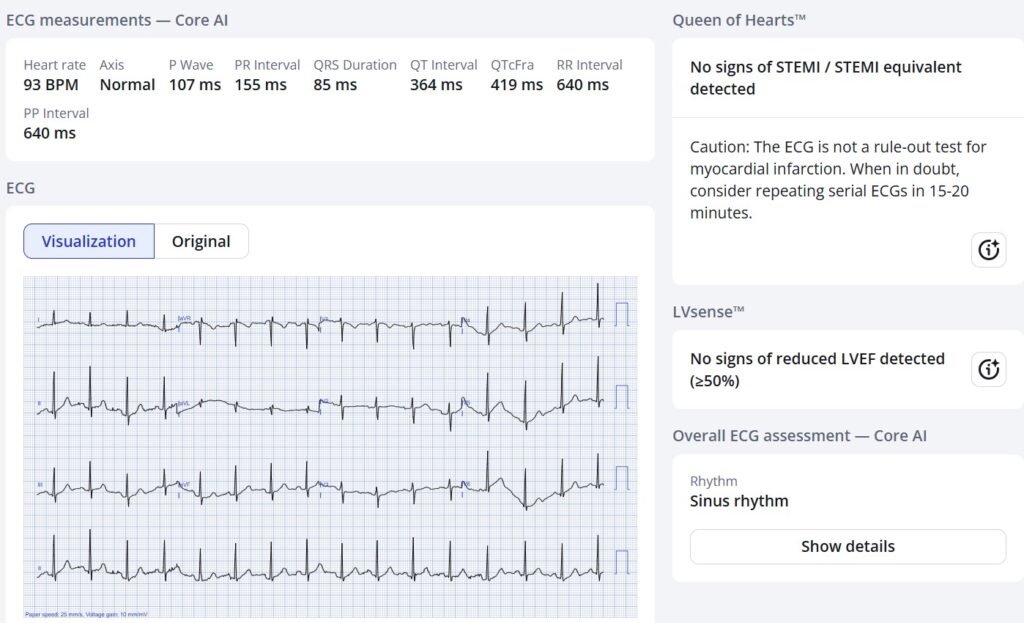
Here is what would happen if you know how to read ECGs, or use the Queen of Hearts:
The presentation ECG shows obvious and diagnostic signs of acute LAD occlusion MI. There are HATW in V2-V5, and some STE (less than STEMI criteria) in V3, V4, II, III, aVF.
Many without training will say there is no reciprocal ST depression on the standard 12 leads (which is true in half of LAD occlusions!), but they are wrong in this case: there is reciprocal STD in aVL from lead III.
If you’re wondering where the reciprocal findings are from the anterior wall, it is quite easy to figure out unless you are brainwashed by the ACC/AHA’s naming convention of the myocardial walls. Where would the opposite of anterior leads be? They would be directly opposite, the posterior leads. The only reason that most anterior STEMIs/OMIs “don’t have reciprocal findings” on the standard 12 lead is because no one gets posterior leads to see the reciprocal findings.
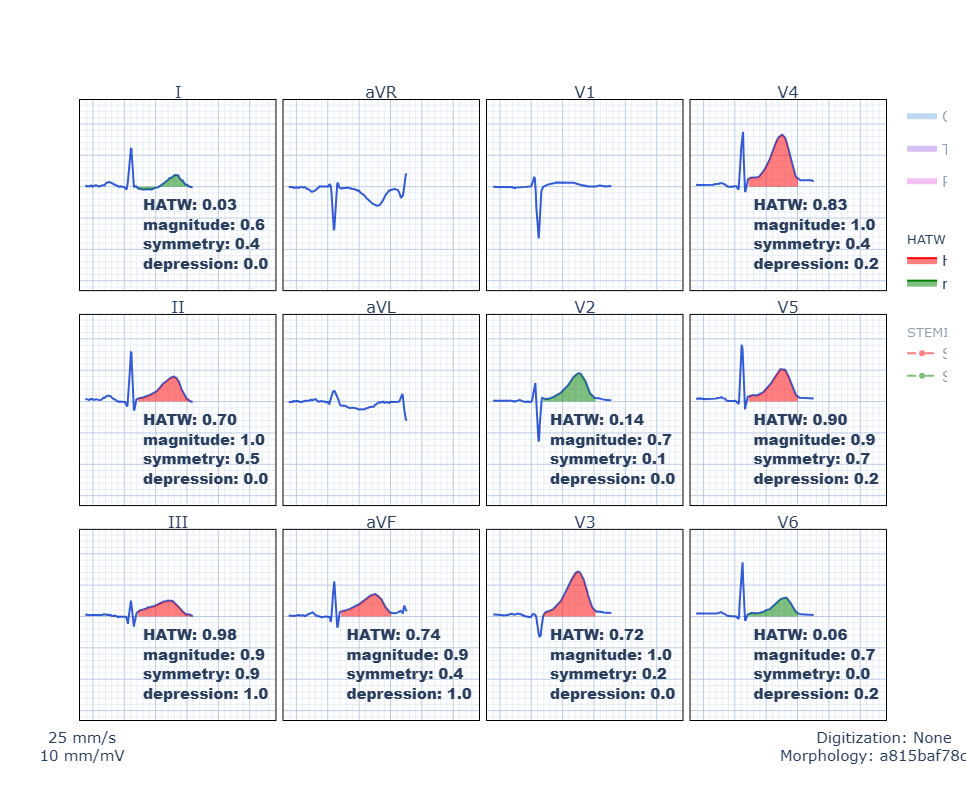
Here is our objective, published HATW score applied to this ECG (red means the T wave meets the HATW criteria):
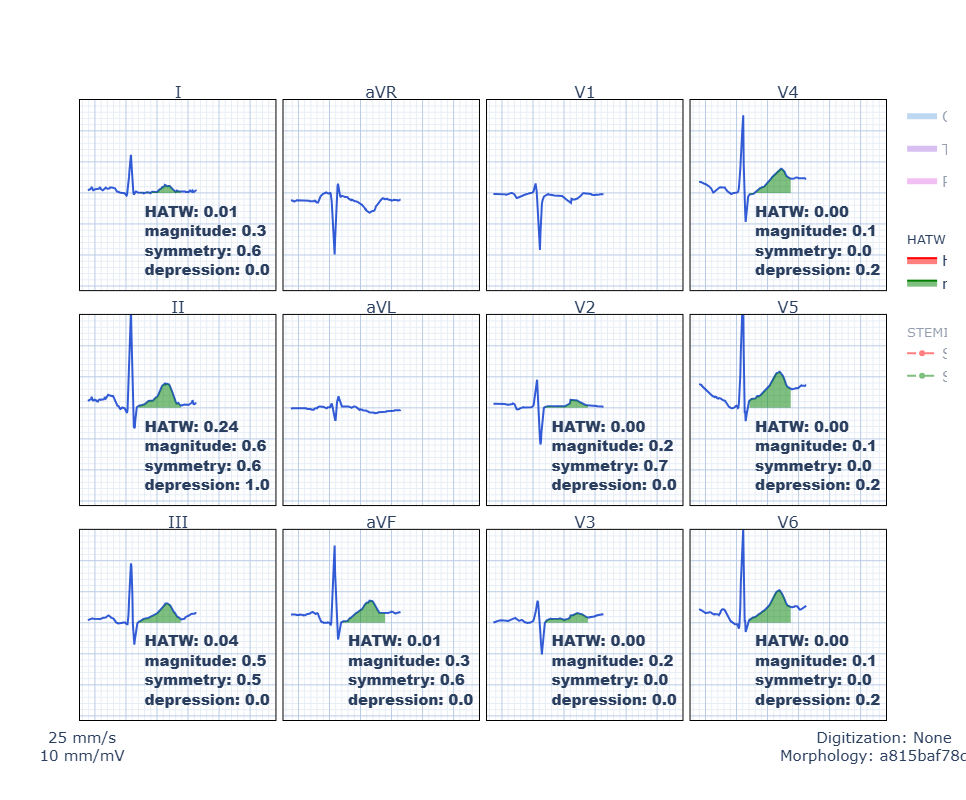
Some may think the Queen just calls everything positive. They are wrong. She has higher specificity than approximately 100% of people who think that, in my experience. Here is her ruling on the baseline ECG (when the patient did not have ACS):
Here is what our formula looks like on the normal baseline ECG without HATWs (green means T waves within normal limits):
Paper where we derived and validate the formula for hyperacute T waves
So what happened to this patient in real life?
Her triage ECG was read as “No STEMI.” And she goes to the waiting room after labs were drawn.
Everyone without good ECG training is surprised when her troponin I returns at 181 ng/L.
So it is a myocardial infarction, but only an NSTEMI.
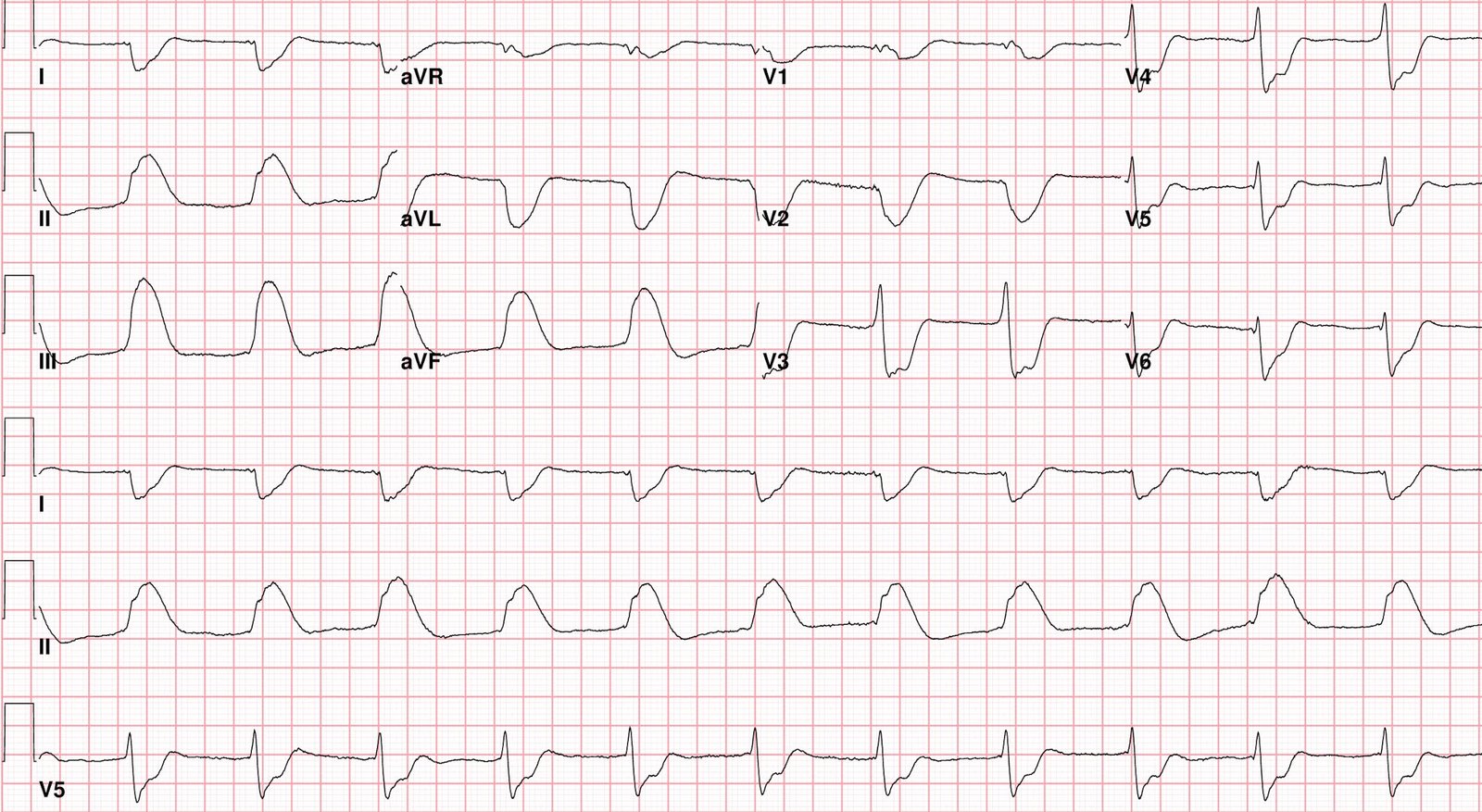
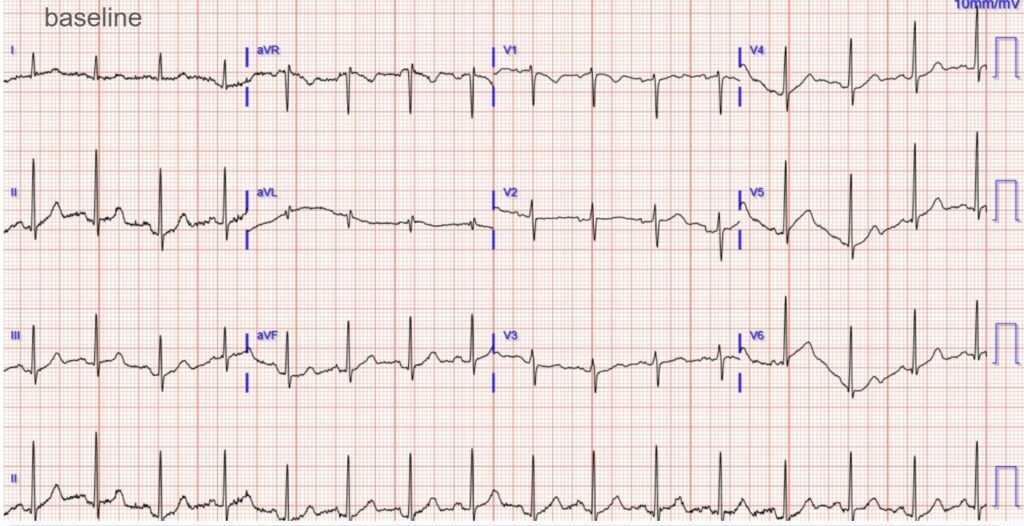
Only then is a repeat ECG ordered (around 2 hours after arrival), despite ongoing pain the whole time:
Now it actually barely meets STEMI criteria in just a few leads. So Queen calls it “STEMI” instead of “STEMI equivalent”, but its just as easy as the first one.
Yet, the normally trained physician did not see any “signs of clear STEMI.” They consulted cardiology who agreed it was “not a true STEMI.” They advised to check a repeat troponin.
Smith: NSTEMI with persistent symptoms are supposed to go emergently to the cath lab as soon as that is discovered. So even if you don’t recognized the acute occlusion on the ECG, the standard of care is to the cath lab. (Of course this standard ALSO leads to unacceptably delayed care — in this case a 2 hour delay, and a 2 hour delay negates most of the benefit of reperfusion.) Anyway, the only study of this showed that these “NSTEMI” guidelines are only followed 6% of the time!
Lupu L, Taha L, Banai A, et al. Immediate and early percutaneous coronary intervention in very high-risk and high-risk non-ST segment elevation myocardial infarction patients. Clin Cardiol [Internet] 2022;Available from: https://onlinelibrary.wiley.com/doi/10.1002/clc.23781The repeat troponin was 368 ng/L.
A repeat ECG was ordered to check for STEMI (around 4 hours in):
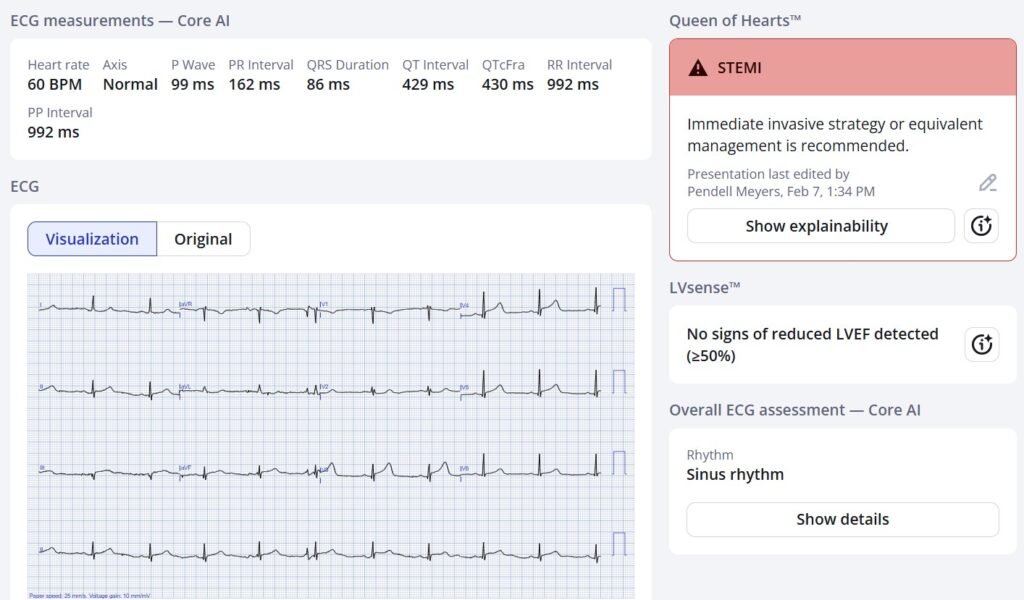
Still it was deemed “not a STEMI”.
She was admitted for “NSTEMI” and given pain medications. The admitting physician re-consulted cardiology when the repeat troponins were >25,000 ng/L.
At about 8 hours after arrival, she had an angiogram performed:
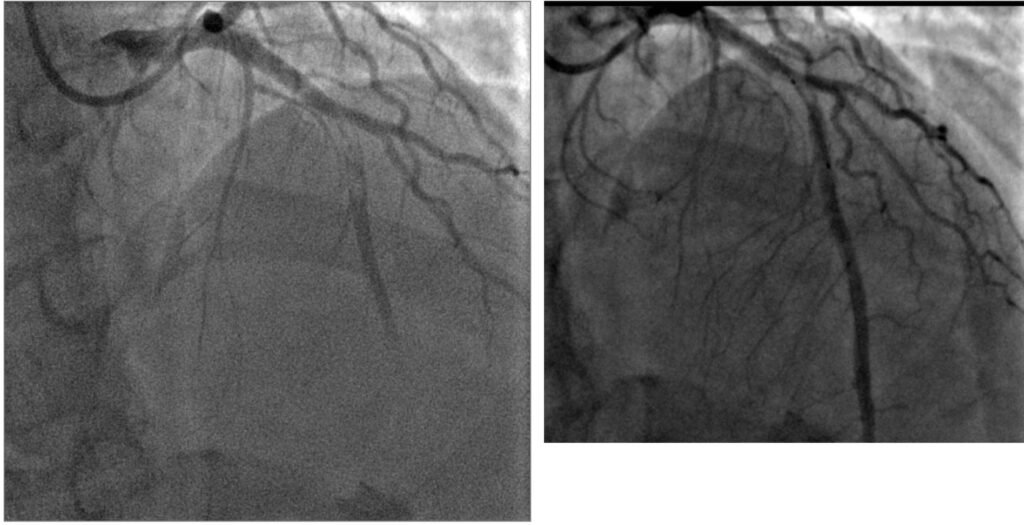
The culprit was described as a total mid-LAD thrombotic occlusion, and she received PCI.
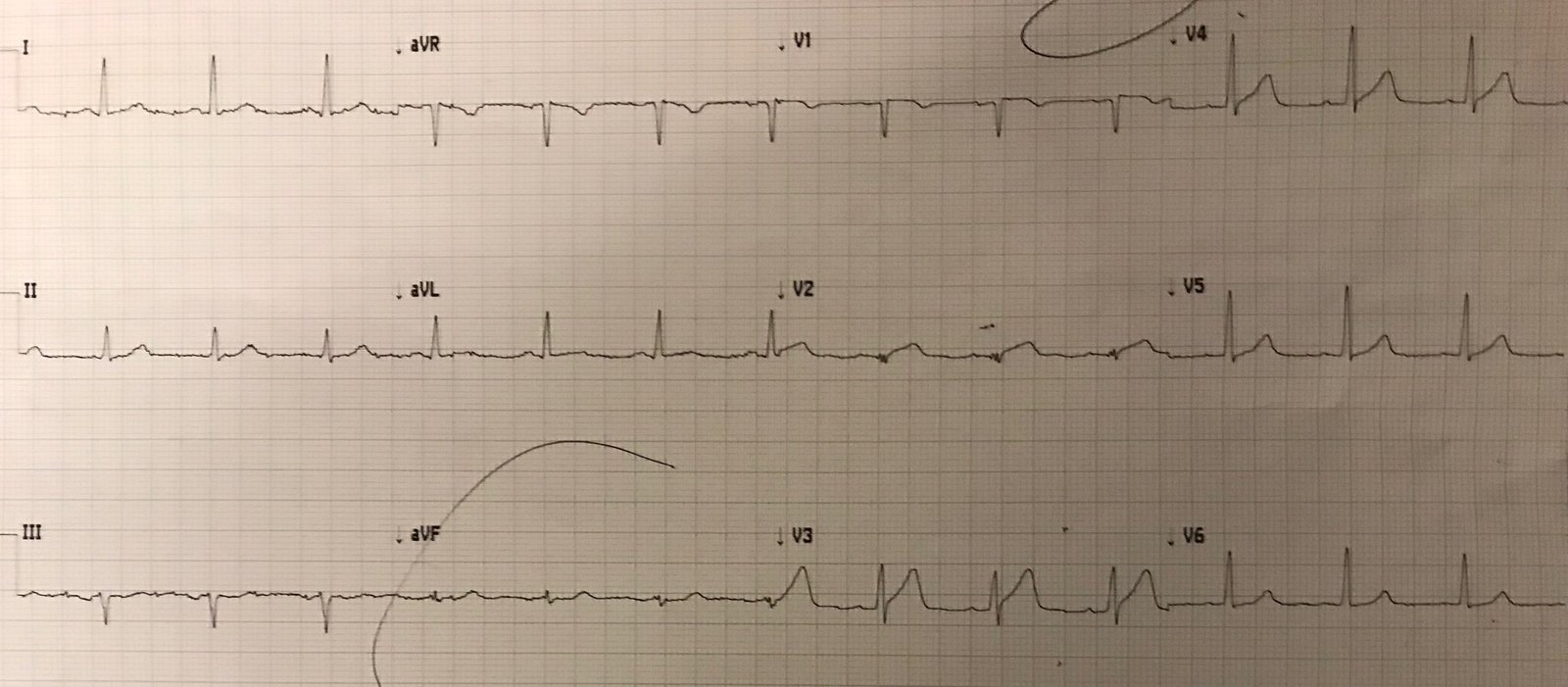
Here is her ECG hours after the PCI:
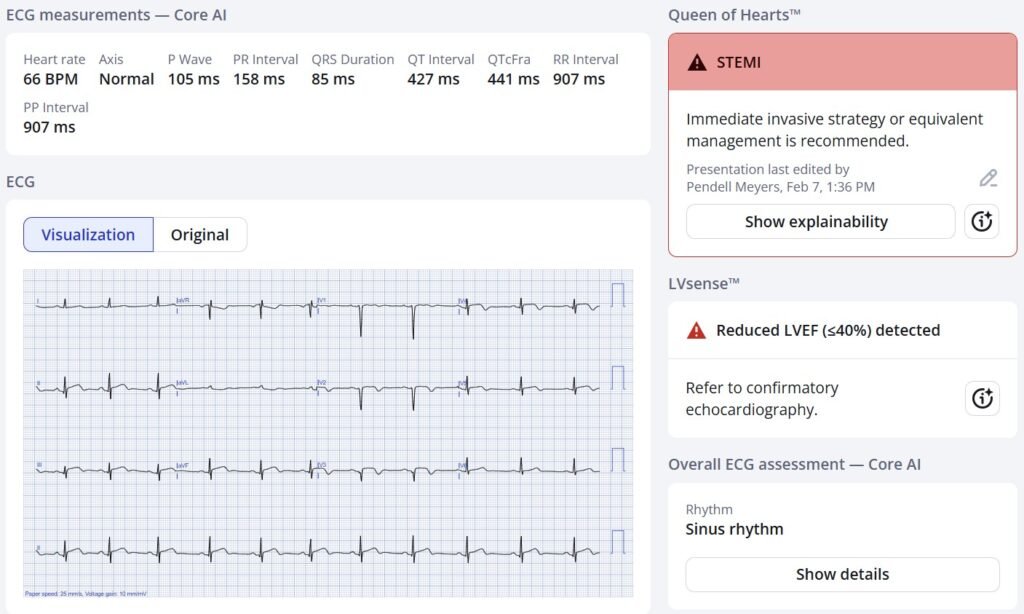
The Queen is trained to be very conservative, so even though our AI models can see there is some reperfusion pattern (terminal to full T wave inversion) occurring in many leads, the Queen still says “STEMI” because she doesn’t know there has been PCI, and there is persistent STE and signs of ongoing ischemia (likely because of the terrible delay to care, resulting in less benefit to intervention).
You can also see that the Queen’s LVEF detection model has detected reduced EF (which was not present in the beginning of her OMI at arrival!).
This was confirmed by formal echo with 37% EF with anterior, septal, and apical WMAs.
She survived the hospitalization, but we know from countless data (see Khan, Wang, etc) that she has a poor long term prognosis compared to AMIs without coronary occlusion (NOMIs). I think the prognosis would be better with immediate reperfusion rather than an 8 hour delay.
Discharge diagnosis: “Acute Non-ST elevation myocardial infarction (NSTEMI) of anterior wall”
She got ACS care of the past (and sadly the present in many places). We are working as fast as we can to change this.
Smith: “NSTEMI” is worthless diagnosis. 30-40% of NSTEMI are Occlusion MI, and they have far worse prognosis than NSTEMI with open arteries, in spite of being younger and healthier at baseline. NEVER diagnose someone with NSTEMI. It is a worthless diagnosis. It has no physiologic or anatomic meaning whatsoever.
New PMcardio for Individuals App 3.0 now includes the latest Queen of Hearts model and AI explainability (blue heatmaps)! Download now for iOS or Android. https://www.powerfulmedical.com/pmcardio-individuals/ (Drs. Smith and Meyers trained the AI Model and are shareholders in Powerful Medical). As a member of our community, you can use the code DRSMITH20 to get an exclusive 20% off your first year of the annual subscription. Disclaimer: PMcardio is CE-certified for marketing in the European Union and the United Kingdom. PMcardio technology has not yet been cleared by the US Food and Drug Administration (FDA) for clinical use in the USA.
= = =
======================================
MY Comment, by KEN GRAUER, MD (2/7/2025):
I found today’s post by Dr. Meyers to be difficult to read. The diagnosis in today’s case should not have been missed (with resultant 8-hour delay in performing cardiac cath with PCI).
- “Time is Muscle (myocardium)”. As emphasized in the October 23, 2025 post (and in the graph Dr. Smith adds to the January 15, 2026 post) — The most benefit from reperfusion occurs within the first 4 hours after acute coronary occlusion (Every 2-hour delay results in 60% more myocardium infarcted).
= = =
In today’s post — Dr. Meyers illustrates in full detail the indisputable virtues of the latest QOH (Queen-Of-Hearts) App 3.0 with AI explainability. Hopefully, at some point in the very near future — insufficiently trained clinicians (including cardiologists) who are still unaware of the OMI paradigm, will at least begin to trust and use the QOH application.
- MY Thought: It should not come to this. That today’s initial ECG so obviously reflects an acute OMI should be readily apparent to any clinician who sees patients with CP (Chest Pain).
- Simple review of no more than a handful of the nearly 2,000 clinical cases that have been posted on Dr. Smith’s ECG Blog since its inception in 2008 should be all that is needed to appreciate (and begin to apply) the basic principles that make the acute OMI in today’s case so obvious!
= = =
How Not to Miss Today’s Diagnosis …
As I highlight in My Comment at the bottom of the page in the January 26, 2026 post of Dr. Smith’s ECG Blog — My List of the 3 KEY factors for simplifying the ECG interpretation of acute OMI rests with attention to: — i) Clinical Context; — ii) Shape; — and, iii) Proportionality. To examine the role of My KEY Factors with respect to today’s case — Consider the following.
- Clinical Context: Today’s patient is a woman in her 40s who came to the ED for new-onset CP. This presentation immediately places her in a higher-risk group for having an acute cardiac event.
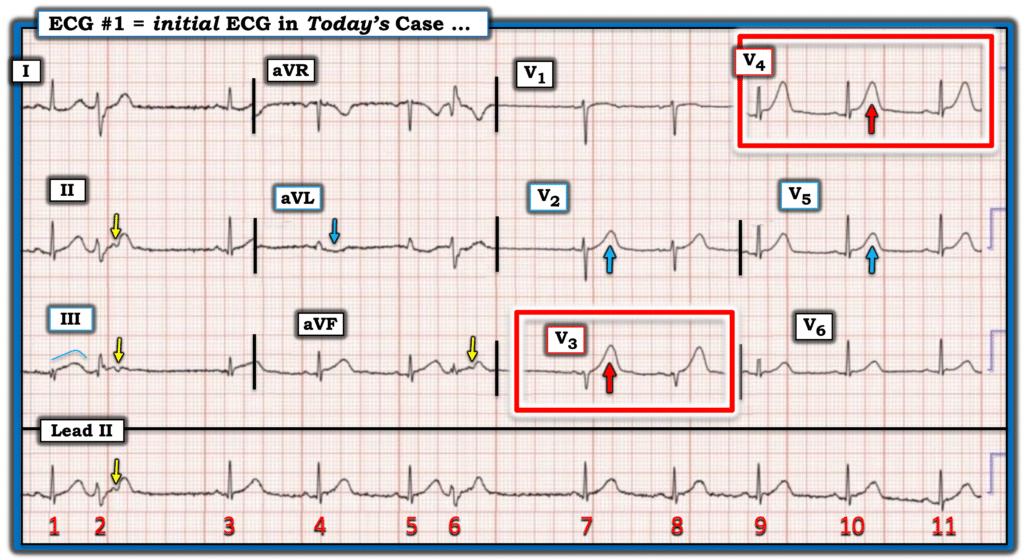
Now consider Figure-1 — in which I’ve reproduced and labeled this patient’s initial ECG.
- The rhythm is Figure-1 is sinus with 2 PVCs. Intervals (PR-QRS-QTc) are normal. The axis is normal. There is no chamber enlargement.
- The Shape of the disproportionately enlarged T waves in leads V3 and V4 (within the RED rectangles in Figure-1) in this patient with new-onset CP — convincingly declare to us that the ST-T waves in both of these leads are hyperacute ( = much “bulkier” and wider-at-their-base, as well as “fatter”-at-their-peak than expected given the small size of the QRS in these leads — most emphatically in lead V3).
- In the Context of knowing that the T waves in leads V3,V4 are clearly hyperacute — neighboring leads V2 and V5, while not as obviously abnormal as leads V3,V4 are — still suggest a continuation of the acute process. The fact that there is loss of R wave from lead V2-to-V3 supports this suggestion that chest lead involvement begins with lead V2.
= = =
Further Proof of Acuity:
- Although more subtle than the ST-T waves in leads V3,V4 — the ST-T wave in lead III is also clearly hyperacute (once again — highlighting the importance of shape and proportionality). Given tiny size of the QRS of beat #1 in lead III — the ST segment of this beat #1 T wave is noticeably straightened, with a “fatter”-than-expected T wave peak, and a disproportionately wide T wave base.
- Unfortunately, the latter part of the ST-T wave of beat #3 in lead III is “cut off” by the lead change that occurs between beats #3 and #4. That said — we do get a glimpse of the ST segment straightening and disproportionately wide T wave base before this lead change occurs — and this confirms our impression that the T wave of beat #1 in lead III is hyperacute.
- Further confirmation of the acuity of the T wave in lead III is forthcoming from the reciprocal ST-T wave depression that we see in lead aVL (BLUE arrow in this lead).
- Finally — there are PVCs! (Premature Ventricular Contractions). While the presence of PVCs is not specific for acute OMI — ventricular ectopy provides yet another sign consistent with acute ischemia.
= = =
Figure-1: I’ve labeled the initial ECG in today’s case.
= = =
In Summary:
To Emphasize — A number of the ECG findings that I highlight above are subtle, and may not be immediately apparent IF viewed in isolation. But, we need to assess today’s initial ECG with attention focused on the 3 KEY factors = i) Clinical Context; — ii) Shape; — and, iii) Proportionality.
- Today’s Clinical Contex is a patient with new CP — which places the patient in a higher-risk group for having an acute cardiac event. This means that even subtle ECG findings take on added importance.
- In a patient with new CP — the principles of Shape and Proportionality immediately define the ST-T waves in leads V3,V4 as hyperacute.
- In the Context of at least 2 definitely hyperacute T waves (in leads V3 and V4) — the less obvious ST-T abnormalities that are seen in at least 5 additional leads add further support to the presence of an ongoing acute OMI until proven otherwise.
What to do at this point should be EASY. In a patient like the woman in today’s case, who presents to the ED with new CP and an initial ECG that shows several hyperacute T waves and a total of at least 7/12 leads with potentially acute ST-T wave findings — a diagnosis of acute OMI is established until proven otherwise (and merits prompt cath). But if providers harbor any doubt at this point about the indication for prompt cath — there are several EASY things to do. These include:
- Acting on the 1st positive Troponin. This should have mandated the need for prompt cath in today’s case.
- Seeking out a prior ECG. On seeing this patient’s previous ECG (that Dr. Meyers showed above) — there can be no doubt that the ECG findings I describe above are acute.
- Repeating the ECG within no more than 10-20 minutes! While sometimes it takes time to manifest ECG evolution of an acute event — Dr. Smith’s ECG Blog is replete with too-numerous-to-count examples of dramatic ST-T wave evolution occurring within minutes of repeating the initial ECG. Development of such “dynamic“ ST-T wave changes is diagnostic of an acute evolving event in need of prompt cath.
- Performing bedside Echo (ie, Finding a localized wall motion abnormality in the context of new-onset CP is diagnostic of an acute event).
Bottom Line: Reading about the events from today’s case is frustrating. Much work remains to continue “spreading the word” that these miscues do not have to be …
= = =
Did You Notice? — Beyond the Core …
While not essential to the diagnosis and management of today’s case — there are some interesting features of the PVCs seen in Figure-1:
- The QRS complex of beats #2 and #6 is not overly wide. While we do not see the appearance of these PVCs in the chest leads (because there are no PVCs after the 2nd lead switch) — QRS morphology of beat #2 in leads I,II,III resembles left posterior hemiblock conduction (rS in lead I — with qR in lead III) — and the wide terminal S waves in leads I and aVL (for beats #2 and 6), together with the tall R wave in lead aVR for beat #6 — suggest right bundle branch block conduction. These features suggest that beats #2 and 6 are fascicular beats arising from the left anterior hemifascicle (with premature fascicular beats portending similar clinical maifestations as PVCs).
- Both of these fascicular beats manifest retrograde P waves ( = the YELLOW arrows in Figure-1). These retrograde P waves reset the SA node, and account for the brief pauses after beats #2 and 6. There is no AV block. (About half of ventricular beats manifest retrograde conduction back to the atria — whereas on-time sinus P waves continue without interruption to “march through” PVCs in the other half).
= = =
= = =
= = =