The source of this case is anonymous.
A 40 something woman with a history of hyperlipidemia and additional risk factors including a smoking history presented with substernal chest pain radiating to “both axilla” as well as the upper back. She was reportedly “pacing in her room while holding her chest”.
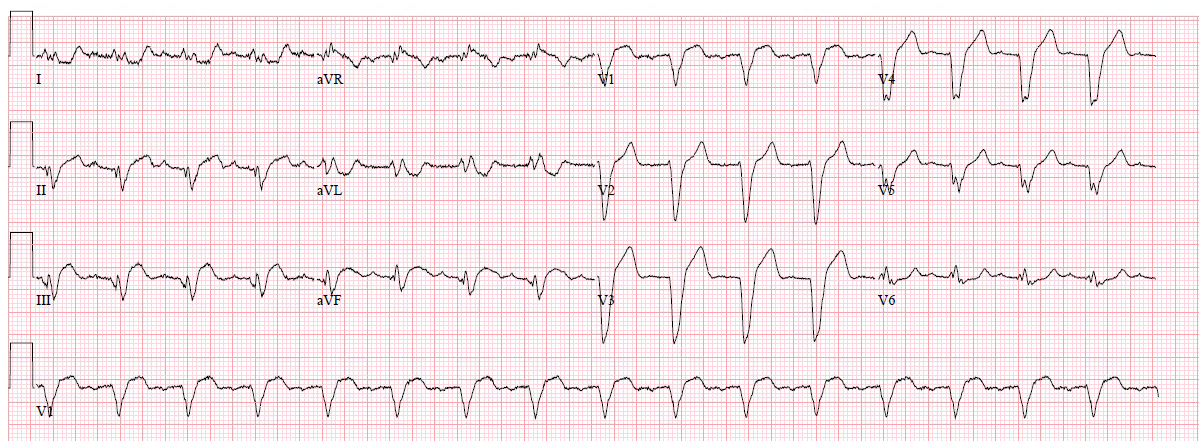
The initial tracing (EKG 1) was obtained.
 |
| Clinician and EKG machine read of acute pericarditis. What do you think? |
There is sinus rhythm. There is diffuse ST elevation in II, III, aVF and V3-V6. One might agree with the computer and the clinician because there is inferolateral ST elevation without any reciprocal ST depression. While it is true that inferior MI has ST depression in aVL 99% of the time (Bischof and Smith), and that inferolateral ST elevation is the most common distribution for pericarditis, the ST elevation in V3 has “terminal QRS distortion (TQRSD),” (diagnostic of LAD occlusion).
Paper published: Terminal QRS distortion not found in any ECG of Early Repolarization
TQRSD is defined as the absence of BOTH an S-wave and a J-wave in leads V2 or V3. While I have shown that early repolarization never has this feature which is common to LAD occlusion, no one has ever studied it in pericarditis. I strongly suspect that pericarditis does not have this feature, and would never assume that it might. When I see this feature, the ECG represents LAD occlusion until proven otherwise.
First, this is so clearly an LAD occlusion that I would simply activate the cath lab. However, if you were prevented from doing that, then an emergent contrast echo is indicated. If there is no wall motion abnormality, then you can be confident that it is not an LAD occlusion.
Why is there diffuse ST elevation (also in inferior leads?). This is almost certainly due to a type 3 (“wraparound”) LAD that supplies the inferior wall.
How about the use of the LAD occlusion formula?
This formula was developed comparing early repol to LAD occlusion, so it may not apply when the DDx is pericarditis vs. LAD occlusion.
1. Forget about diagnosing pericarditis here; it is too rare and it is too dangerous to diagnose it in lieu of MI.
2. Much of what is called pericarditis is really early repolarization.
See this case, written by Pendell Meyers when he was a student:
31 Year Old Male with RUQ Pain and a History of Pericarditis. Submitted by a Med Student, with Great Commentary on Bias!
3. TQRSD is a sign of obvious LAD occlusion. These cases were excluded from the study that derived and validated the formulas, and so you should not rely on the formula when there is TQRSD. Just diagnose LAD occlusion!
Nevertheless, here are the values if you use the formula:
QTc = 431, STE60V3 = 2 mm, RAV4 = 5 mm, QRSV2 = 5 mm
3-variable: 26.2 (greater than 23.4 is LAD occlusion)
4-variable: 22.4 (greater than 18.2 is LAD occlusion)
Clinical course
Later, the first troponin I returned at 2.67 ng/mL (quite elevated).
Comment: If you are still somehow convinced that this ECG represents pericarditis, then you must at least change your diagnosis to myo- pericarditis (because the elevated troponin shows myocyte necrosis). But in patients with ST elevation due to myocarditis, there will be a wall motion abnormality and elevated troponin, so it usually can’t be differentiated from MI without an angiogram.
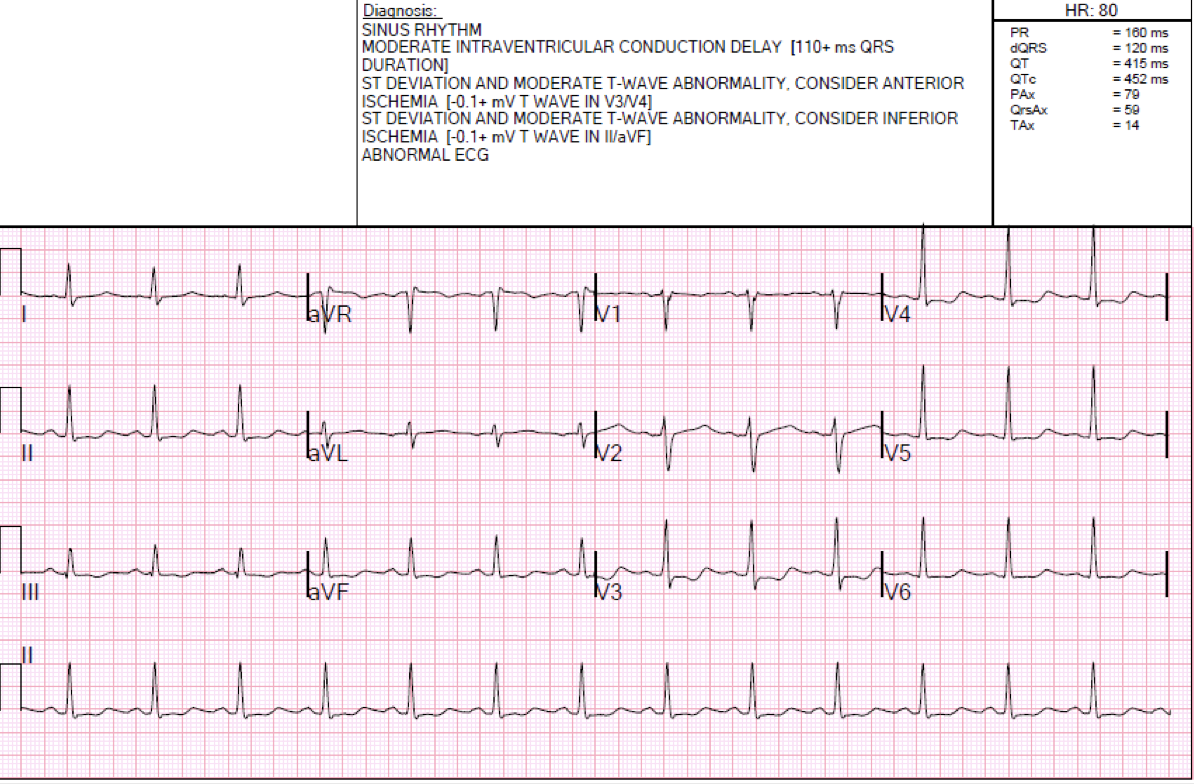
Another ECG was recorded:
 |
| Is it true that there is “no significant change”? |
In the intervening 3 hours, new Q-waves have developed in leads V3 and V4, and deepened in V5 and V6.
The patient was admitted to medicine service for pericarditis where she had intermittent pain throughout the rest of the night. The medicine note documents that the patient had worsening pain with lying flat and relief with leaning forward. There was no history of preceding viral symptoms.
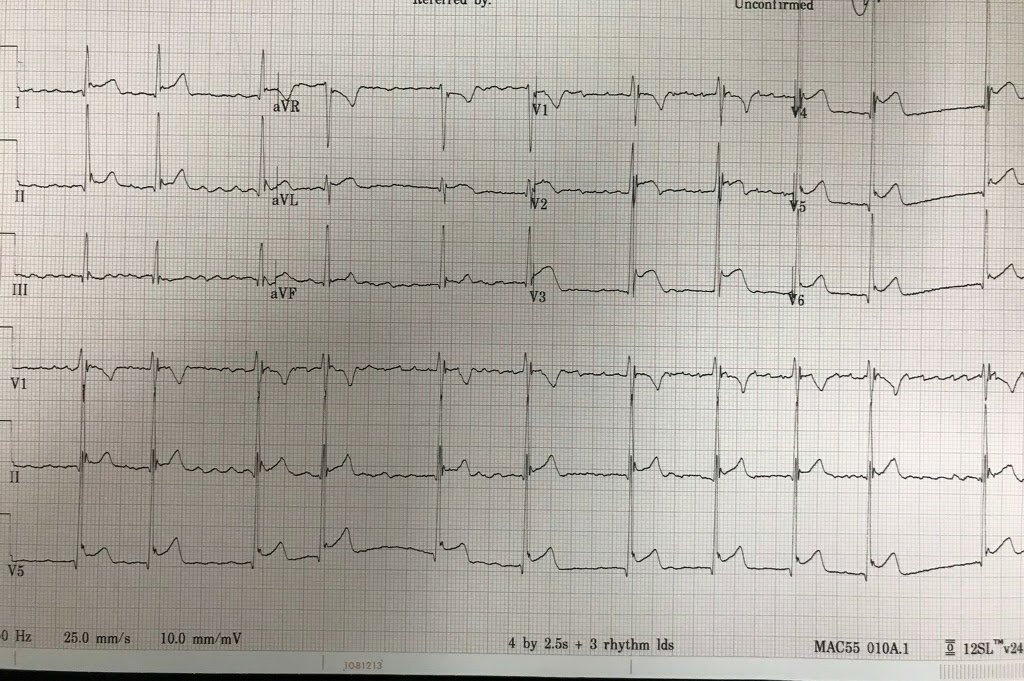
Another ECG was recorded at t = 6 hours:
 |
| The Q-waves are more pronounced and now the computer sees it. Also, the ST elevation has diminished as myocardium infarcts |
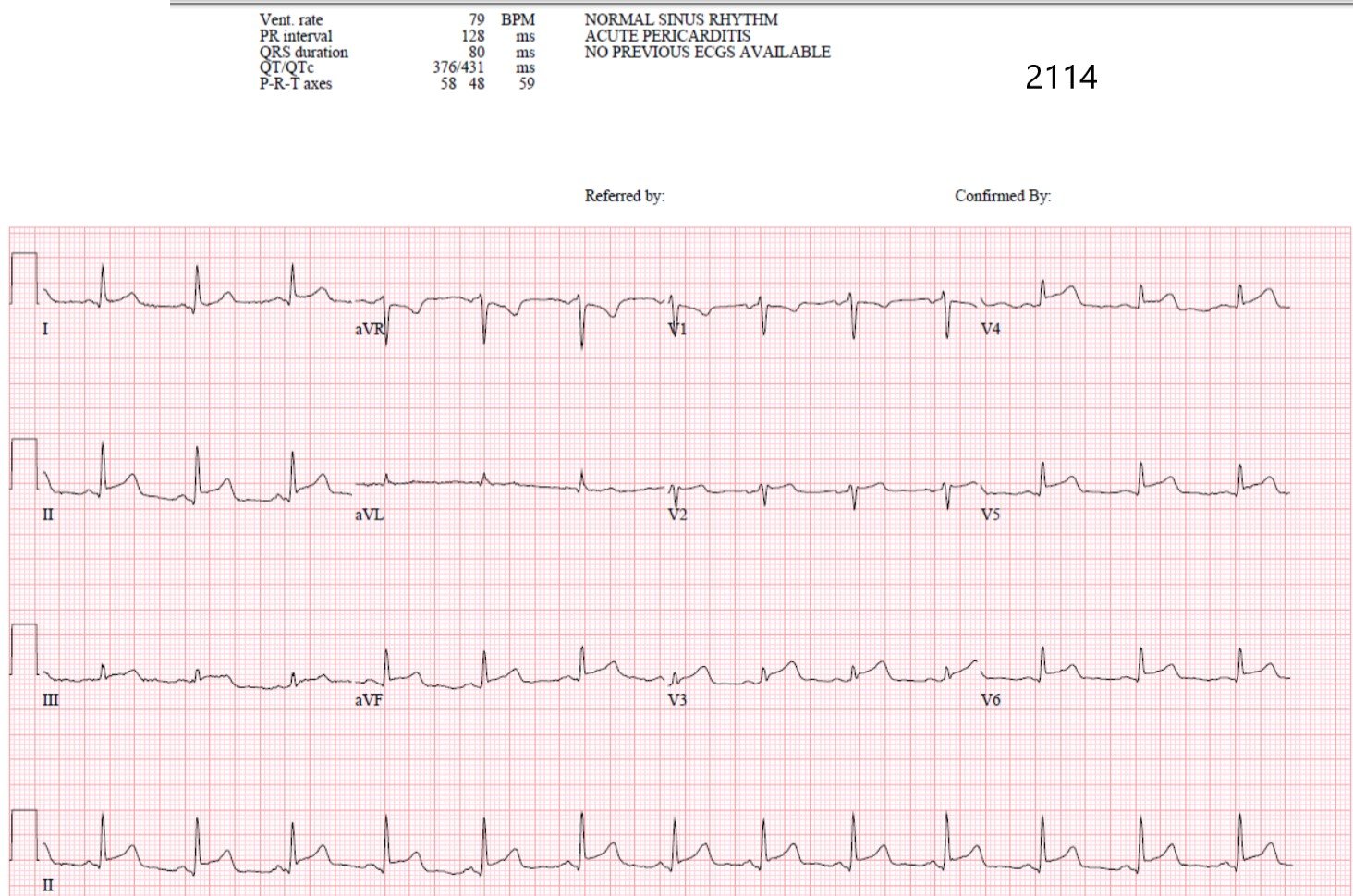
Outcome and comments by the source of the case:
“The following morning the cardio consult service saw the patient. The repeat TnI at that time was 19.20 ng/mL and an official echo showed: ‘Severe hypokinesis to akinesis of the apical 1/3 anteroseptal wall with partial wall thinning c/w apical anterospetal MI.'”
“Cath showed a 100% mid LAD lesion which was successfully intervened upon.”
“TnI peaked at 67.10 ng/mL post PCI.”
“I know from reading your blog that you “diagnose pericarditis at your own peril”, but are there any signs on that initial ECG that would make you think ischemia? No PR depression, no Spodicks sign, but concave segments which are diffusely elevated… no reciprocal depressions (aVL looks isoelectric to me, maybe make an argument for slight depression?).”
“In the clinical context I would have performed a bedside echo and had I seen the RWMA the diagnosis would have been made, but in the absence of this I thought that initial ECG looked like pericarditis.”
2 comments:
1. 40-50% of acute LAD occlusion have upwardly concave ST segments in all of V2-V5.
–Smith SW. Upwardly
Concave ST Segment Morphology Is Common in Acute Left Anterior Descending
Coronary Artery Occlusion. Journal of Emergency Medicine 2006;
31(1):67-77.
2. 40-50% of LAD occlusion have zero reciprocal ST depression.
–>