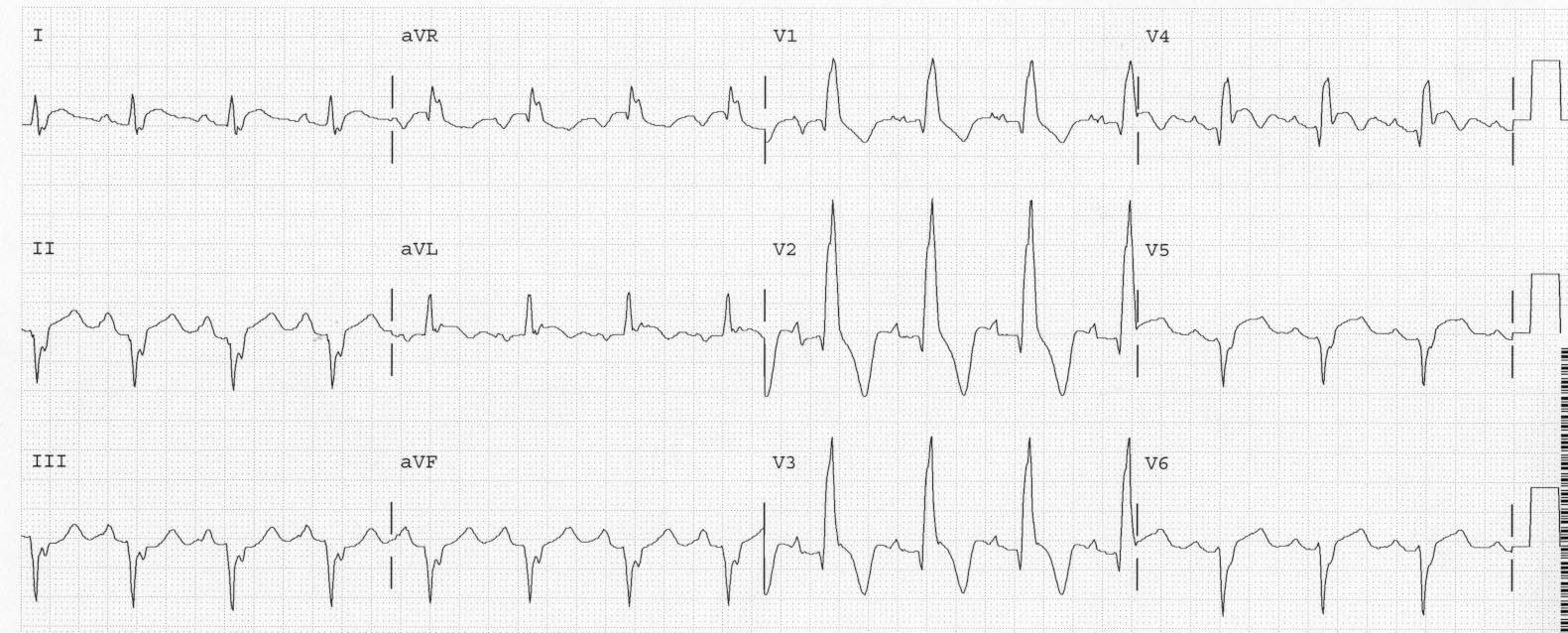
History: This woman in her 20’s (age) with history of
repaired Tetralogy of Fallot presented with CP. Here is her presenting ECG:
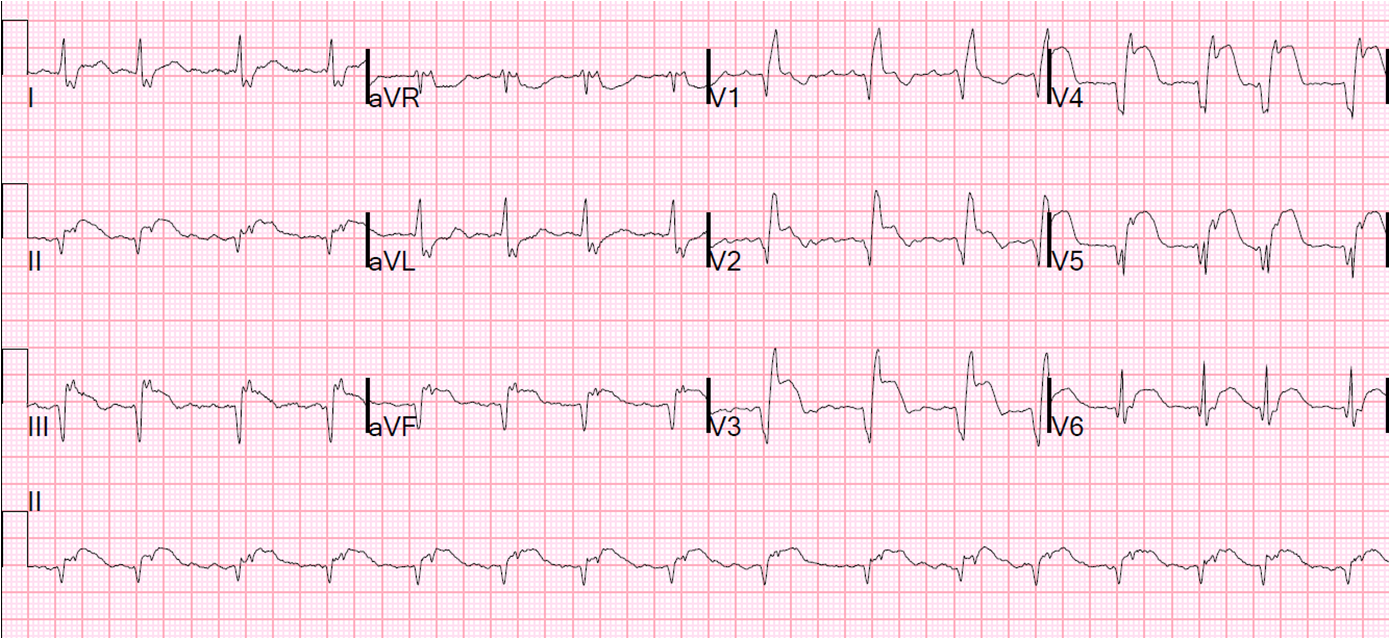
I was very suspicious of anterior STEMI, and found a previous ECG from 4 months prior:
 |
| Very large RR’ in V1: RBBB and RVH, also LAFB
Baseline ST depression in V1-V3, typical for RBBB. There is no ST elevation anywhere, also typical for RBBB. |
So there is relative ST elevation in V2 (relative to the previous ST depression) and new ST elevation elsewhere.
An
immediate echo confirmed new anterior-apical-septal wall motion
abnormality, as well as RVH and LVH, and the patient was taken for
angiography, which revealed fresh non-occlusive thrombus in the left
main that extended down and occluded the LAD. The patient went for
bypass surgery.
Lessons:
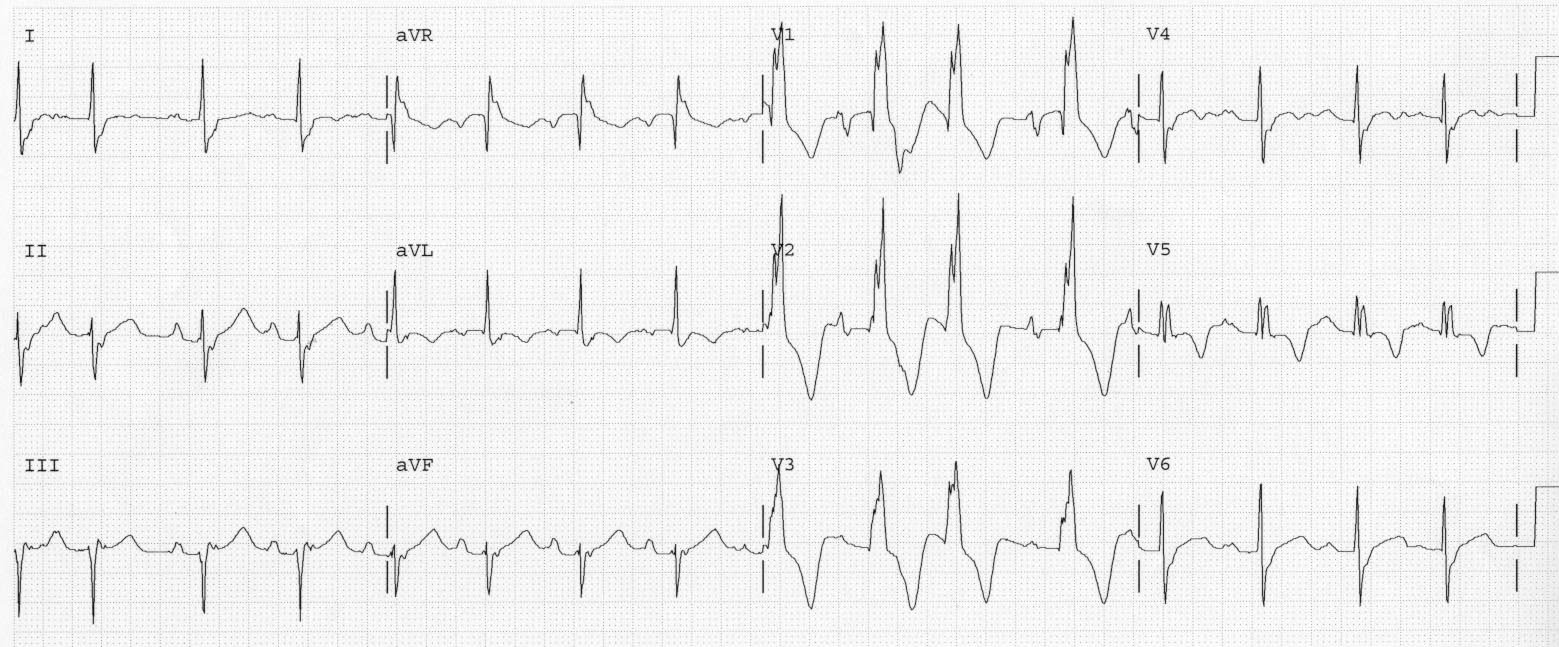
1. RBBB should not have ST elevation at baseline
2. In RBBB, there should be some ST depression in V2 and V3. An isoelectric ST segment may represent relative ST elevation.
3. A previous ECG can be very helpful
4. Echocardiography did confirm the findings, but delayed therapy. The ECG was diagnostic.
5. ST elevation can be found even when the QRS
appears very distorted.