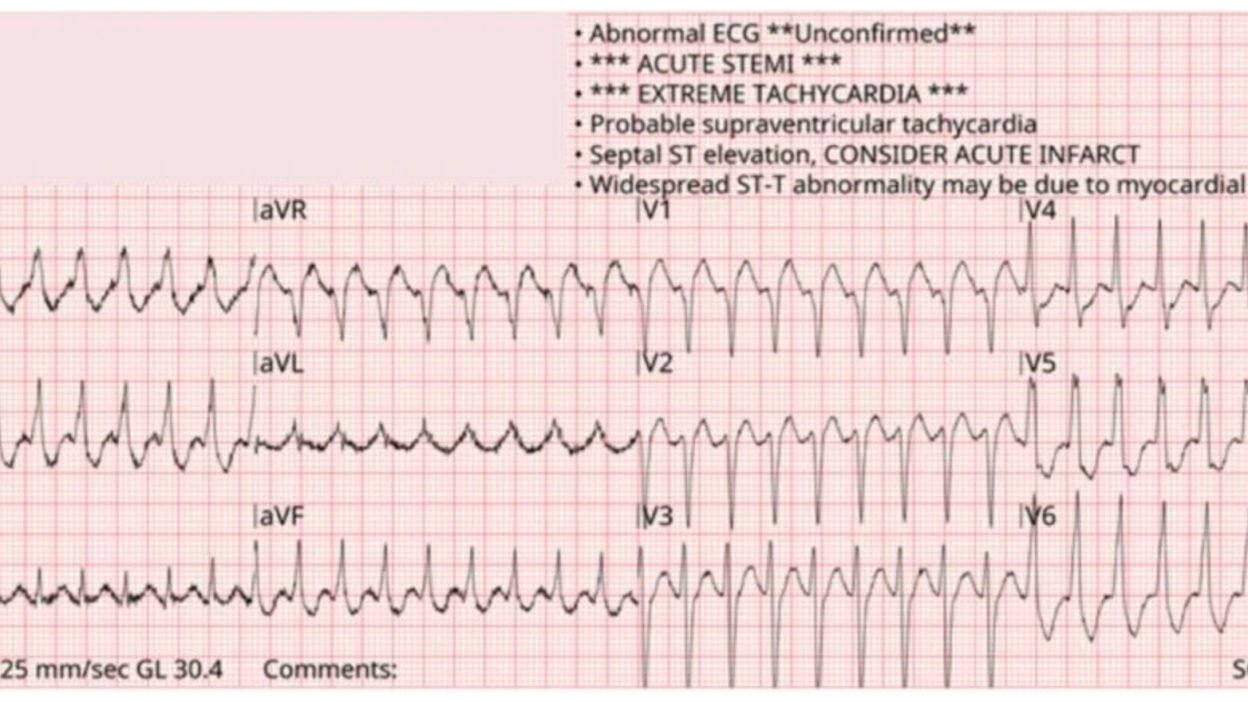
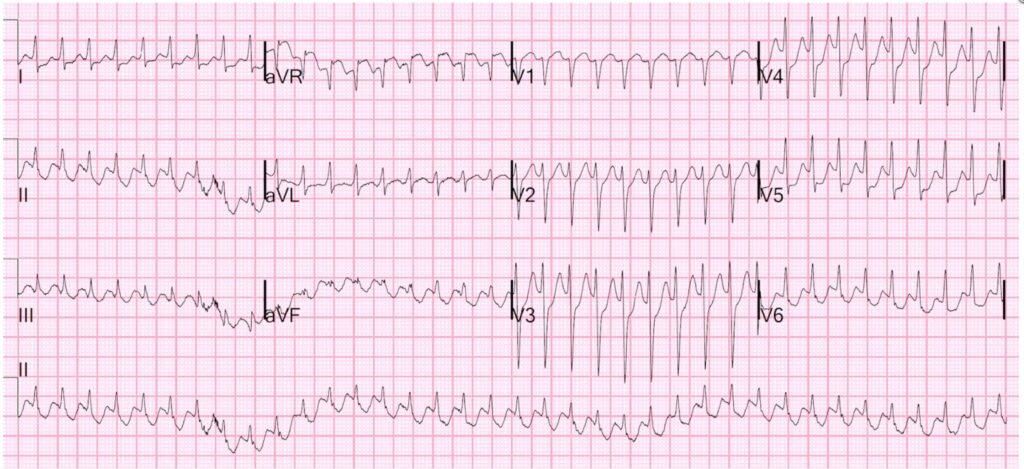
A 53 year old man with paroxysmal atrial fibrillation and multiple myeloma called EMS with chest discomfort and palpitations. When paramedics arrived, they found him awake and alert and said his chest felt “off.” 12-lead ECG is shown.

What do you think?
When a patient has hemodynamically unstable tachycardia, cardioversion is always reasonable. The EMS report indicates blood pressure 144/59 mmHg, respiratory rate 16, oxygen saturation 99% breathing ambient air. So no immediate need for cardioversion.
What’s our differential diagnosis? The very fast rate (~212 bpm) forces us to consider ventricular tachycardia. However, the QRS duration is not particularly wide, less than 100 ms. Therefore supraventricular tachycardia is much more likely.
Smith: when the rate is very fast, you should always be CERTAIN that it is regular. Very fast atrial fib, which is always irregularly irregular can, at first glance, appear to be regular. This one is indeed regular.
In addition, the RR interval is quite regular. The differential diagnosis for regular SVT is:
- Sinus tachycardia
- Atrioventricular nodal reentrant tachycardia (AVNRT)
- Atrioventricular reentrant tachycardia (AVRT)
- Atrial tachycardia (AT)
- Atrial flutter (AFL)
- Junctional tachycardia (JT – rare, I will not discuss it in this post)
Sinus tachycardia is perhaps the most important to recognize, as sinus tachycardia is physiologic and should not be treated with rate slowing medications. Imagine a patient with a massive pulmonary embolism and compensatory sinus tachycardia whose heart rate is slowed with a beta blocker. They could easily die.
Once sinus tachycardia has been ruled out, consider the tools available to us and what impact they would be expected to have: Vagal maneuvers, adenosine, and AV nodal blockers – chiefly calcium channel blockers (CCB) and beta blockers (BB).
Vagal maneuvers
The REVERT randomized trial taught us that modified vagal maneuvers increase the likelihood of successful termination of SVT. This is accomplished by putting the patient in a semi-recumbent position, having them strain (e.g. by blowing into a syringe) for 15 seconds, and then laying them flat and raising their legs to 45° as described in this video.
When it works to terminate SVT, it does so by blocking conduction through the AV node with increased vagal tone. Therefore, it stands a good chance at terminating the tachycardias which involve the AV node as part of the circuit. Which ones are those? AVNRT and AVRT. What will transient suppression of the AV node do to AT or AFL? Nothing. (Except perhaps transiently slow the ventricular rate.)
CCBs/BBs
As with vagal maneuvers, these drugs work by suppressing conduction through the AV node. Hence they are often able to terminate AVNRT and AVRT.
But in addition, they can suppress automaticity! For this reason, they often slow or terminate AT (if it is due to automaticity). They may lower the rate of ventricular conduction in atrial flutter, but it is notoriously difficult to rate control and therefore CCBs/BBs may do nothing at all to AFL.
Adenosine
As with vagal maneuvers and CCBs/BBs, adenosine transiently blocks all conduction through the AV node. It is complete heart block in a bottle. Fortunately, the effects only last a few seconds. What will it do to each tachycardia?
AVNRT/AVRT: Typically terminate
AFL: No impact on the flutter circuit, but temporary inhibition of AV conduction which will slow the ventricular rate long enough to clearly show the underlying flutter waves. So although it is not therapeutically useful, it can still be diagnostically useful if the rhythm is unclear.
AT: Complicated! It depends on the mechanism of arrhythmia and a detailed discussion is beyond the scope of this post. I will summarize by saying most atrial tachycardias are not terminated by adenosine. More on this here.
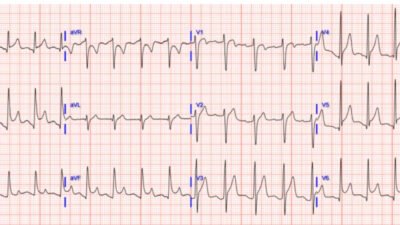
Smith: this is my slide on Atrial Tachycardia:

To summarize
Vagal maneuvers, adenosine, and CCBs/BBs will almost never make any SVT worse, but may have no impact. So what are the downsides to each? With vagal maneuvers, there is almost no downside. The downside of adenosine is primarily that it makes patients feel awful. Serious adverse events are quite rare. The downside of CCBs/BBs is that it may not terminate the rhythm and you could get stuck with hypotension with a longer half-life drug (vs adenosine which is gone in seconds).
Smith: be VERY careful with CCBs if the ejection fraction is low. Electricity is much preferred, and if there is recurrence, try amiodarone.
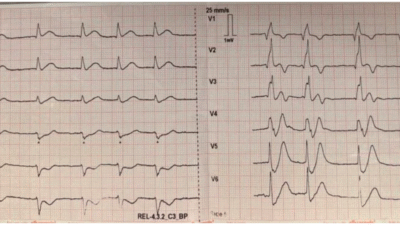
This is summarized in the table below:

Back to the case
This patient received several doses of adenosine. We do not have any recordings, but documentation indicates that it briefly terminated the rhythm before it re-initiated. This is a suspicious story, and it is more likely that this is simply not a rhythm that terminates with adenosine. In this patient’s case, review of his medicines revealed that he was taking flecainide, a crucial bit of information.
Flecainide is commonly used for rhythm control of atrial fibrillation, and it works in part by slowing cardiac conduction. One known risk with flecainide is the possibility of atrial flutter with 1:1 conduction. Why is this?
The typical (atrial) rate for atrial flutter is 300 beats per minute. Thanks to the protective abilities of the AV node, the fastest the ventricle will ever beat is with 2:1 conduction, meaning 300/2 = 150 beats per minute. But because flecainide slows conduction, the atrial rate could drop a bit lower, e.g. to 240 beats per minute. This might be at a rate where the AV node is actually able to accommodate 1:1 conduction. So although the atrial rate is actually slower, this paradoxically produces dangerously fast ventricular conduction.
For this reason, any patient on a class 1C agent (flecainide or propafenone) should ALWAYS also be on an AV nodal blocker to reduce the likelihood of 1:1 flutter.
Case conclusion:
Upon arrival to the ER, the patient underwent synchronized cardioversion with restoration of normal sinus rhythm. Flecainide was washed out and he was started on amiodarone for rhythm control and referred for outpatient ablation.
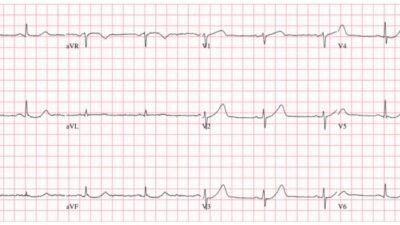
Sinus rhythm ECG is shown below:

Note that the QRS on the flutter ECG was slightly widened with slurring of the upstroke relative to the sinus rhythm ECG. This is because of a property of flecainide known as “use dependence,” where its effect is more pronounced at higher heart rates.
Learning points:
- For hemodynamically unstable SVT, cardiovert
- For hemodynamically stable SVT, it is always reasonable to start with a modified vagal maneuver
- The choice of adenosine vs CCB/BB is at the discretion of the treating clinician, but I prefer adenosine due to its short duration of action
- Flecainide can predispose to atrial flutter with 1:1 conduction
Smith: More amazing related cases:
See this VERY instructive case of flutter with 1:1 conduction that spontaneously “converted” (Not!!): Narrow Complex Tachycardia at a Rate of 220.
What happens when you give adenosine to a patient with this rhythm?

Wide complex tachycardia at a rate of 270

Several Wide Complex Rhythms in One Patient. Test yourself: Will You See What I Did Not See?

And more cases of flecainide and atrial flutter.
= = =
======================================
MY Comment, by KEN GRAUER, MD (9/26/2025):
Today’s case by Dr. Frick reviews the differential diagnosis of a regular SVT (SupraVentricular Tachycardia) rhythm, in which clear sign of atrial activity is absent. I’ll add the following thoughts to Dr. Frick’s review.
- Attention to the ventricular rate may prove invaluable in working through the diagnostic possibilities for a regular SVT rhythm that Dr. Frick notes. Although exceptions exist — sinus tachycardia in a non-exercising adult rarely exceeds ~170/minute. Therefore — the rate of 212/minute for today’s initial tracing makes sinus tachycardia highly unlikely.
- Note: All bets are off in children — who may manifest sinus tachycardia at rates in excess of 200/minute.
- The rate of 212/minute in today’s tracing also makes “untreated“ AFlutter highly unlikely. As per Dr. Frick — the typical rate for flutter waves in an adult is ~300/minute (with the usual flutter rate range being between ~250-350/minute). As a result — I immediately discounted “untreated” AFlutter in my differential diagnosis, since 212/minute is too fast for 2:1 AV conduction with AFlutter — and too slow for 1:1 AV conduction IF the AFlutter is “untreated”.
- All bets are off with “treated” AFlutter. This highlights the KEY point that the accuracy of our differential diagnosis depends on knowing IF the patient in front of us is on any antiarrhythmic medication. Awareness of this point should have prompted inquiry about any rate-slowing medication that today’s patient might have been taking.
- We should suspect that today’s patient may have indeed been on some antiarrhythmic medication given the history of PAF (Paroxysmal AFib) — when we noticed that he is now presenting with a regular SVT rhythm, despite his history of AFib.
- In my experience — hard copy recording during the 60-to-90 or so seconds that Adenosine is active is all-to-often not done. In my opinion — this defeats the diagnostic benefit of this amazing medication. Adenosine almost always works for the reentry SVT rhythms ( = AVNRT; AVRT) — but with other SVT etiologies, the transient rate reduction produced by Adenosine usually reveals the underlying mechanism of the arrhythmia, even though it may not restore sinus rhythm. The effect is fast, and likely to be missed unless you make a 60-to-90 second hard copy recording during the period of maximal Adenosine action. Hard copy allows you then to go back and study the recording — in which you will almost always find clues to the arrhythmia’s true mechanism.
- 1:1 AFlutter at 212/minute is a perfectly logical conclusion to today’s interesting case. But a picture is worth 1,000 words — so proof of 1:1 AFlutter was most probably revealed but lost in those recordings that we unfortunately do not have.