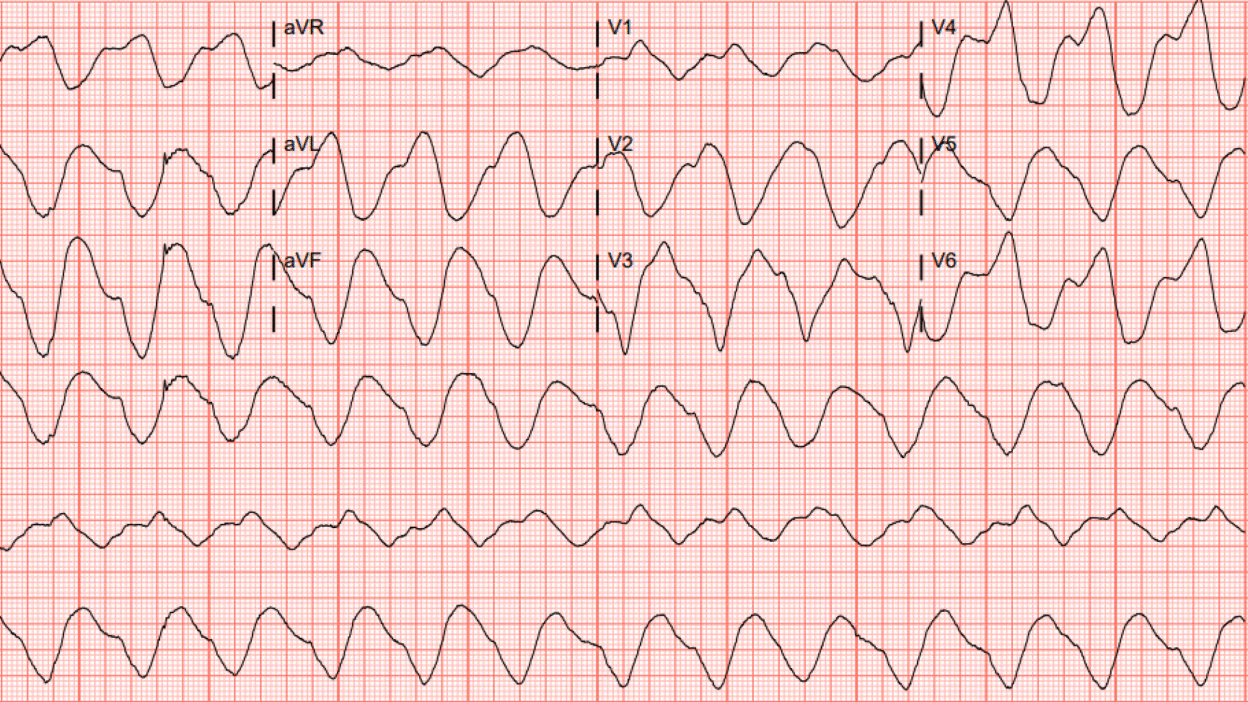
50 year old male with PMH of ESRD, heart failure, pancreatitis and previous MI presents to the ED with chief complaint of epigastric pain. He was described as “altered” with limited history able to be obtained due to mental status on arrival. Here is his triage ECG:
What are your initial thoughts? – This EKG looks sinusoidal and highly concerning for hyperkalemia – Wide complex – Rate too slow to be Vtach
Patient then divulges that he has not been dialyzed in 5 days, hyperkalemic treatment started with albuterol, insulin, dextrose, loklema and only 2g calcium gluconate.
(Meyers note: this is a common and important initial mistake, 2g calcium gluconate is not nearly enough for this peri-arrest hyperkalemia).
Smith: remember that to equal 1 “amp” of Calcium chloride, you must give 3 of calcium gluconate. That is the molar equivalent, since the molecular weight of gluconate is far larger than that of chloride.
Initial K returned at 8.4 mEq/L
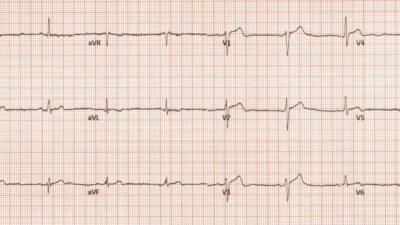
Repeat EKG shortly after initial treatment:
This ECG looks even worse than the first! 2gm calcium gluconate was not enough. This was realized, and next 6 more gm of calcium gluconate were given.
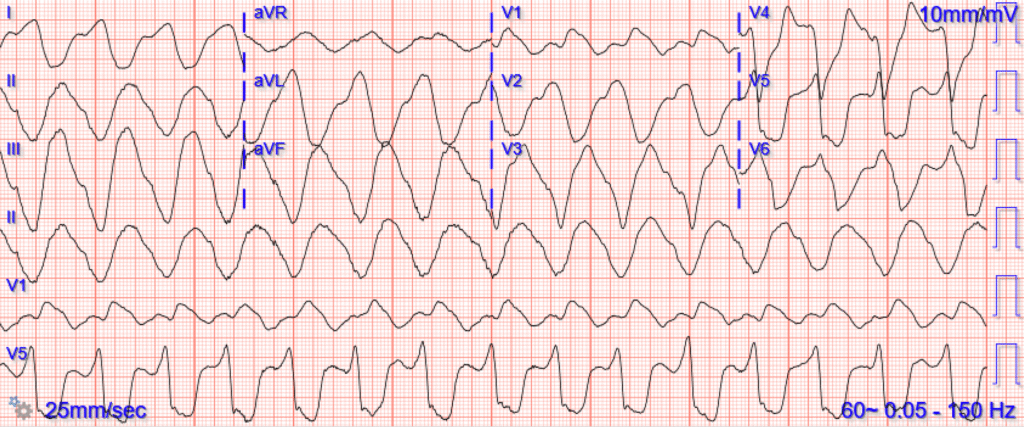
Here is the ECG shortly after that:
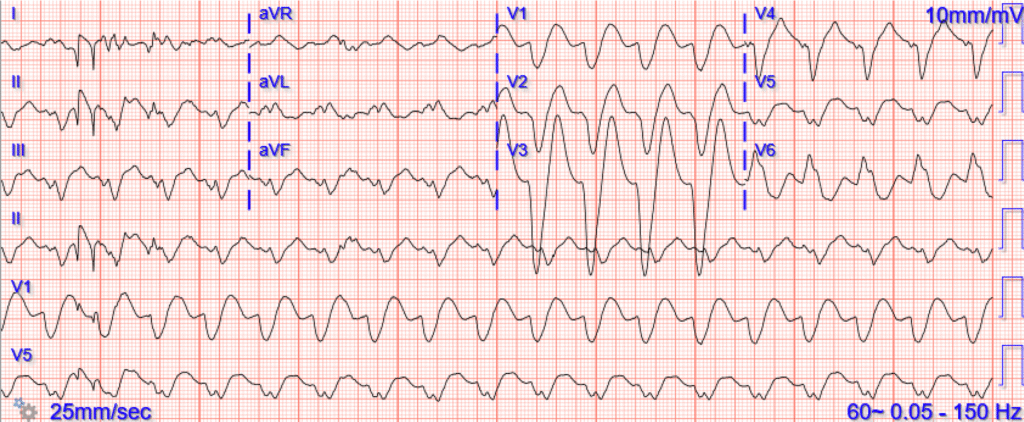
As hoped, the QRS has improved somewhat, the rate has increased, and P waves have become more clear.
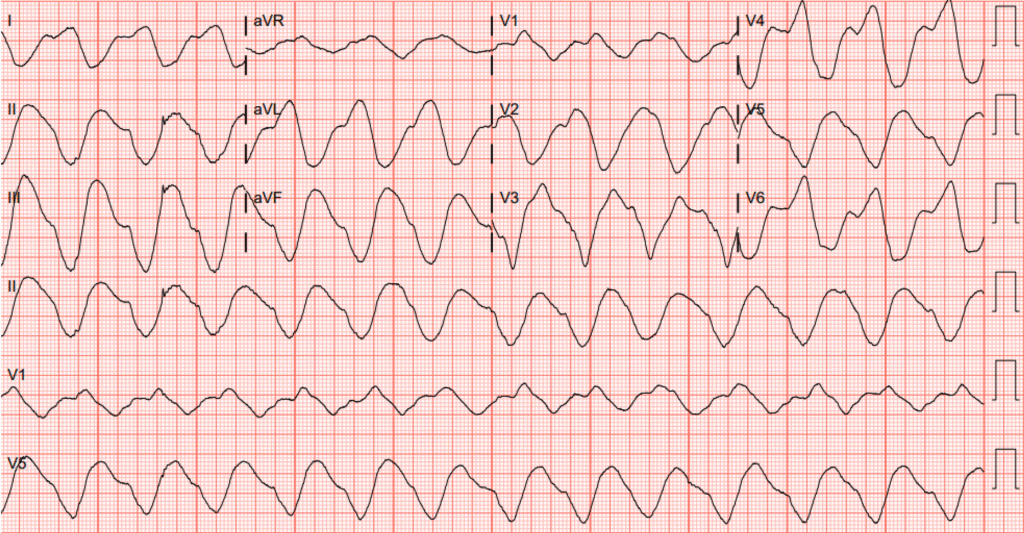
The patient underwent dialysis and a repeat EKG was obtained:

The QRS has narrowed. There is likely underlying LVH, maybe also LAFB. The most concerning hyperkalemic findings have resolved.
The patient did well.
In this case, the providers thought that 1 g of calcium gluconate had fixed the hyperK. But what really happened? Tachycardia and hyperkalemia. What will happen after therapy with 1 gram of Ca gluconate and some bicarbonate?
General hyperkalemia cases:
A 50s year old man with lightheadedness and bradycardia
Patient with Dyspnea. You are handed a triage ECG interpreted as “normal” by the computer. (Physician also reads it as normal)
Severe shock, obtunded, and a diagnostic prehospital ECG. Also: How did this happen?
A woman with near-syncope, bradycardia, and hypotension
What happens if you do not recognize this ECG instantly?
A woman in her 50s with dyspnea and bradycardia
A patient with cardiac arrest, ROSC, and right bundle branch block (RBBB).
Is this just right bundle branch block?
Is This a Simple Right Bundle Branch Block?
A 60-something who has non-specific generalized malaise and is ill appearing.
HyperKalemia with Cardiac Arrest.
Peaked T waves: Hyperacute (STEMI) vs. Early Repolarizaton vs. Hyperkalemia
What will you do for this altered and bradycardic patient?
I saw this computer “normal” ECG in a stack of ECGs I was reading
What is the diagnosis?
Found comatose with prehospital ECG showing “bigeminal PVCs” and “Tachycardia at a rate of 156”
An elderly woman found down with bradycardia and hypotension
A middle aged man with unwitnessed cardiac arrest
Test almost all of your most important ECG rhythm interpretation skills with this case.
Sinus rhythm with a new wide complex QRS
This ECG is pathognomonic and you must recognize it.
A Very Wide Complex Tachycardia. What is the Rhythm? Use Lewis Leads!!
A Very Wide Complex
Are these peaked T-waves the patient’s baseline T-waves?
Bradycardia, SOB, in a Dialysis Patient
Cases of hyperkalemia mimicking OMI:
Acute respiratory distress: Correct interpretation of the initial and serial ECG findings, with aggressive management, might have saved his life.
“Steve, what do you think of this ECG in this Cardiac Arrest Patient?”
Hyperkalemia and ST Segment Elevation, Post 1
A Tragic Case, related to the last post
A patient with chest pain and ST Elevation in V1 and V2
You MUST recognize this pattern, even if it is not common
ST Elevation. What is it?
This ECG Pattern Told the Story When the Patient Could Not
What are these ST elevations, ST depressions, and tall T waves diagnostic of?
Another Shark Fin. With a twist.
Do you recognize this ECG yet?
Right Bundle Branch Block with ST Elevation in V1?
ST elevation in aVL with reciprocal ST depression in the inferior leads
Shock, bradycardia, ST Elevation in V1 and V2. Activate the Cath Lab?
Another deadly and confusing ECG. Are you still one of the many people who will be fooled by this ECG, or do you recognize it instantly?
= = =
======================================
MY Comment, by KEN GRAUER, MD (12/23/2025):
Today’s case by Dr. Meyers brings home a series of important points about the ECG appearance and management of hyperkalemia.
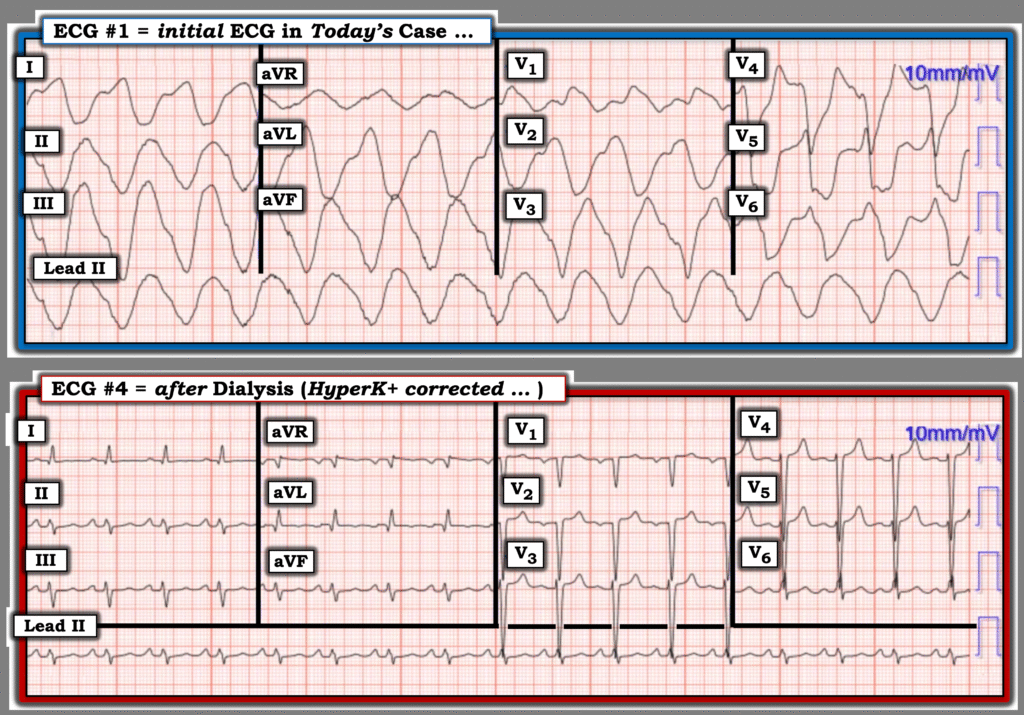
- For clarity in Figure-1 — I’ve reproduced the 1st and last ECG recorded in Dr. Meyers discussion.
= = =
Figure-1: The 1st and last ECG recorded in today’s case:
= = =
The Need for Instant Recognition and Treatment:
The “ECG picture” in Figure-1 — should instantly tell you that some toxicity is operative. Once you verify that the recording speed is 25 mm/sec. (and not 50 mm/sec.) — you will know that this ECG appearance is the result of some toxicity (which most commonly is hyperK+) until proven otherwise because:
- i) The QRS is so wide that I don’t even know how to measure it.
- ii) The QRS is of an amorphous (totally formless) morphology.
As per Dr. Meyers — the importance of instant recognition of this “ECG picture” — is not to delay treatment because you are awaiting lab confirmation of the serum K+ level. Instead — Immediately treat with IV calcium gluconate (realizing that 2 gm IV Ca++ gluconate may not be enough to stabilize the patient in this life-threatening situation).
- The “beauty” regarding clinical management of this pre-lethal serum K+ level (as shown above by Dr. Meyers with sequential ECGs) — is that you’ll know within minutes if you are giving enough IV Ca++ by progressive improvement in ECG parameters.
- iii) BONUS: Once we learn that today’s patient has ESRD (End-Stage Renal Disease), and that he has not been dialyzed for 5 days — any doubt about hyperkalemia is removed. But the point to emphasize is that even without this incriminating history — empiric treatment of ECG #1 with as much IV Ca++ as is needed to narrow the QRS and return this initial tracing to a recognizable ECG morphology is indicated (and essential for optimal outcome).
= = =
The Post-Dialysis Tracing:
I think it insightful to compare side-by-side the 2 ECGs in Figure-1:
- ECG #4 (recorded after medical treatment of hyperkalemia — and after dialysis) — now shows sinus rhythm P waves, with a narrow QRS, and really no indication of hyperkalemia. T waves in the chest leads are upright, and although slightly peaked — these T waves are not pointed — and the upstroke and downstroke of these T waves is not symmetric (as it tends to be with hyperkalemia). I would not have known this patient had life-threatening serum K+ elevation hours earlier from this ECG #4.
- As is common (and expected) in a patient with ESRD — this patient clearly has LVH (Peguero Criteria citing that the sum of the deepest S in any chest lead + the S in V4 far exceeds the required 28mm for LVH).
- NOTE: Criteria for LVH can be conveniently accessed from the Menu at the top of every page in Dr. Smith’s ECG Blog ==> CLICK HERE to see how to find this information.
= = =
Additional Learning Point:
- In the presence of significant hyperkalemia — You will often have no idea as to what the ECG will look like until hyperkalemia is corrected. This applies not only to the marked LVH that today’s patient has — but more important, acute OMIs may be masked by hyperkalemia — which is why it is essential to always repeat the ECG after correcting hyperkalemia.
= = =
= = =