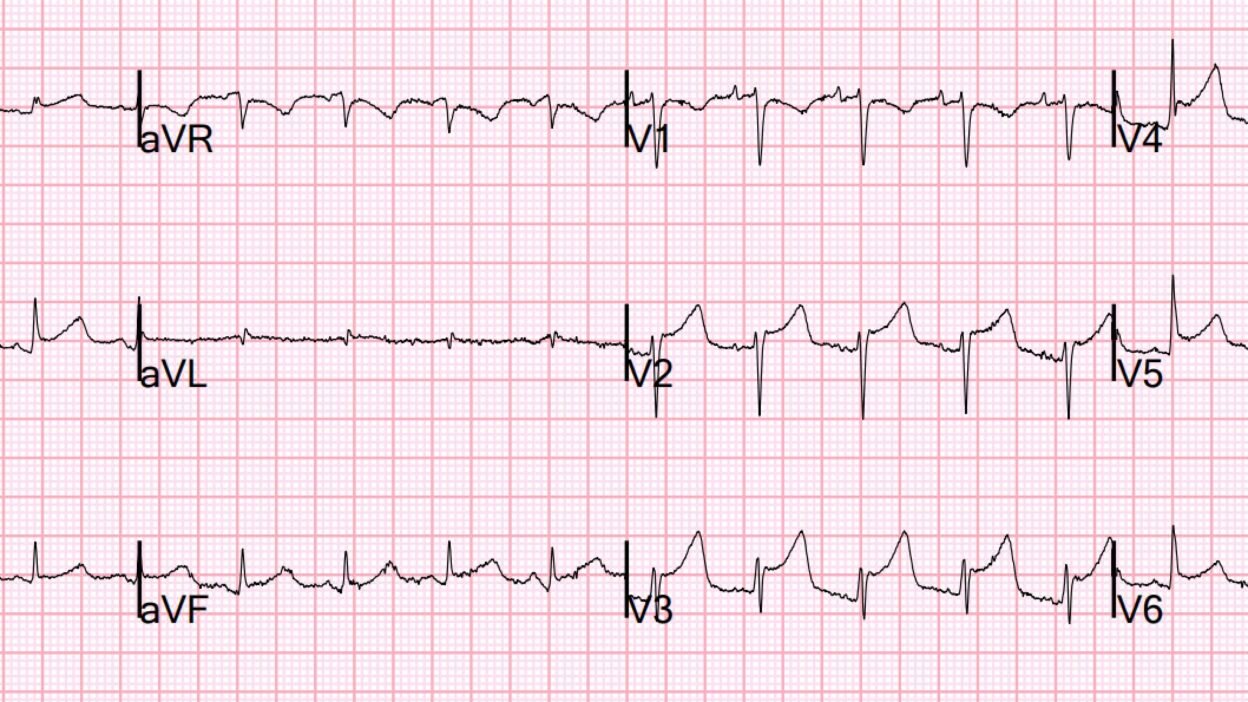
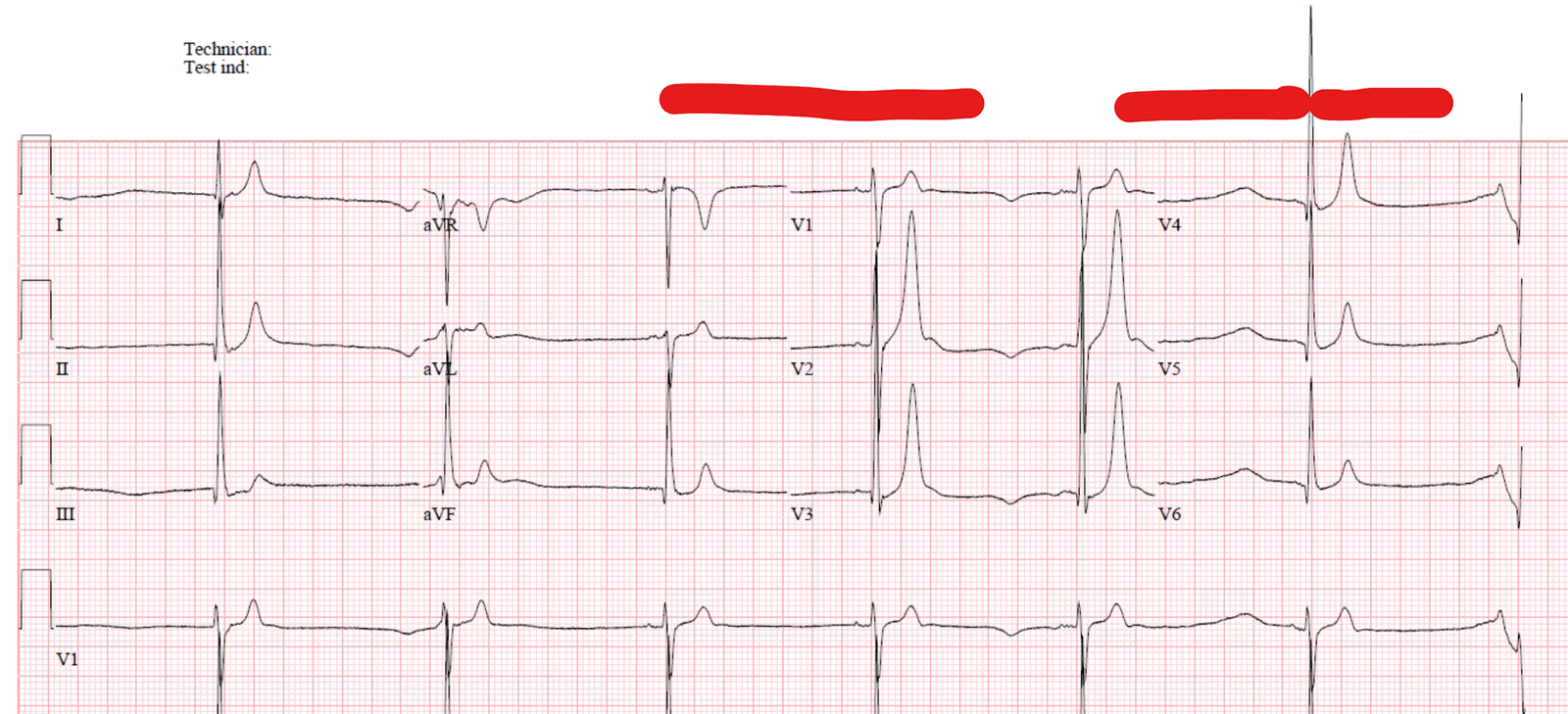
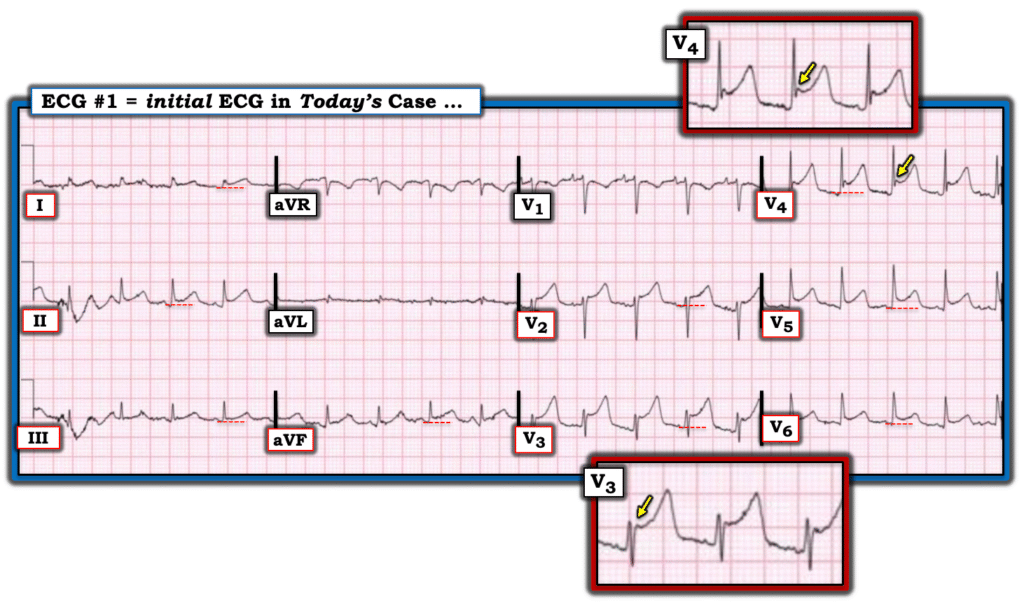
An elderly male presented to the ED with need for G-tube replacement. This was done, and an abdominal X-ray was done to confirm placement. This included much of the chest, and showed a pleural effusion and pulmonary edema. Due to pulmonary edema, an EKG was recorded:

What do you think?
The Queen of Hearts always asks this:
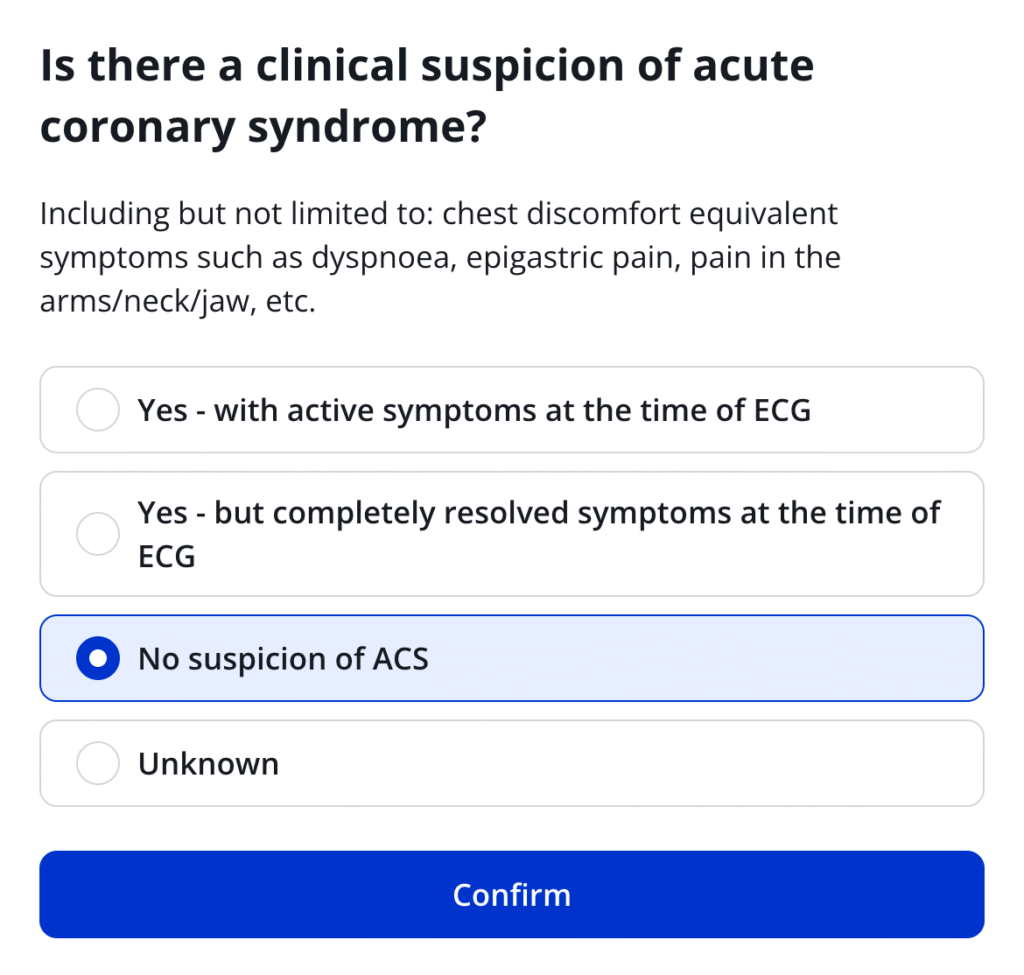
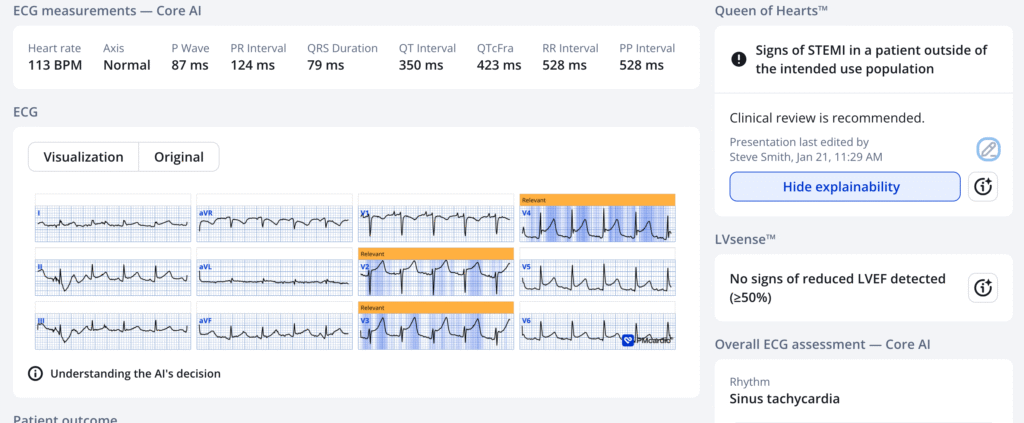
Here is the Queen of Hearts interpretation if we answer that there is “No suspicion:”
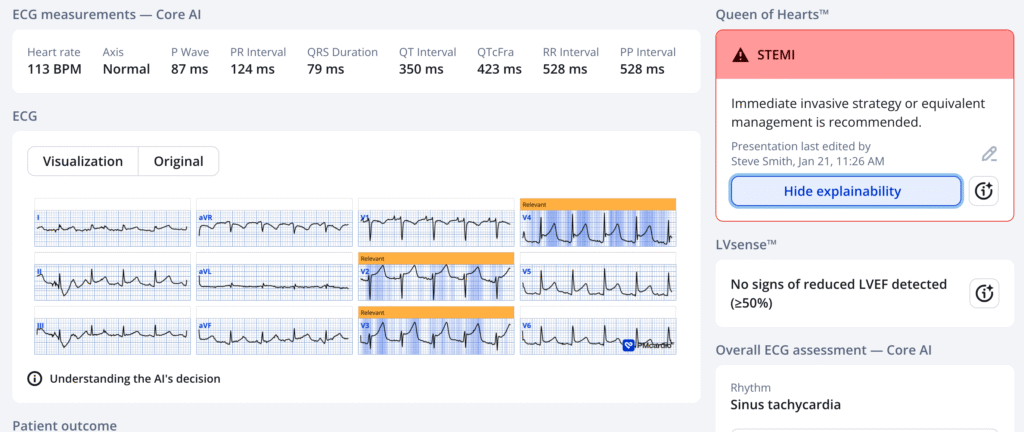
Here is what she would have said if we answered “yes”:
I was shown this ECG in real time and I said:
This could be OMI or could be pericarditis. Is there any history of tumor infiltration into the pericardium? The answer was unknown. I said, “Just do a bedside echo. If this is OMI there should be a large wall motion abnormality. If there is an effusion, then it is pericarditis.
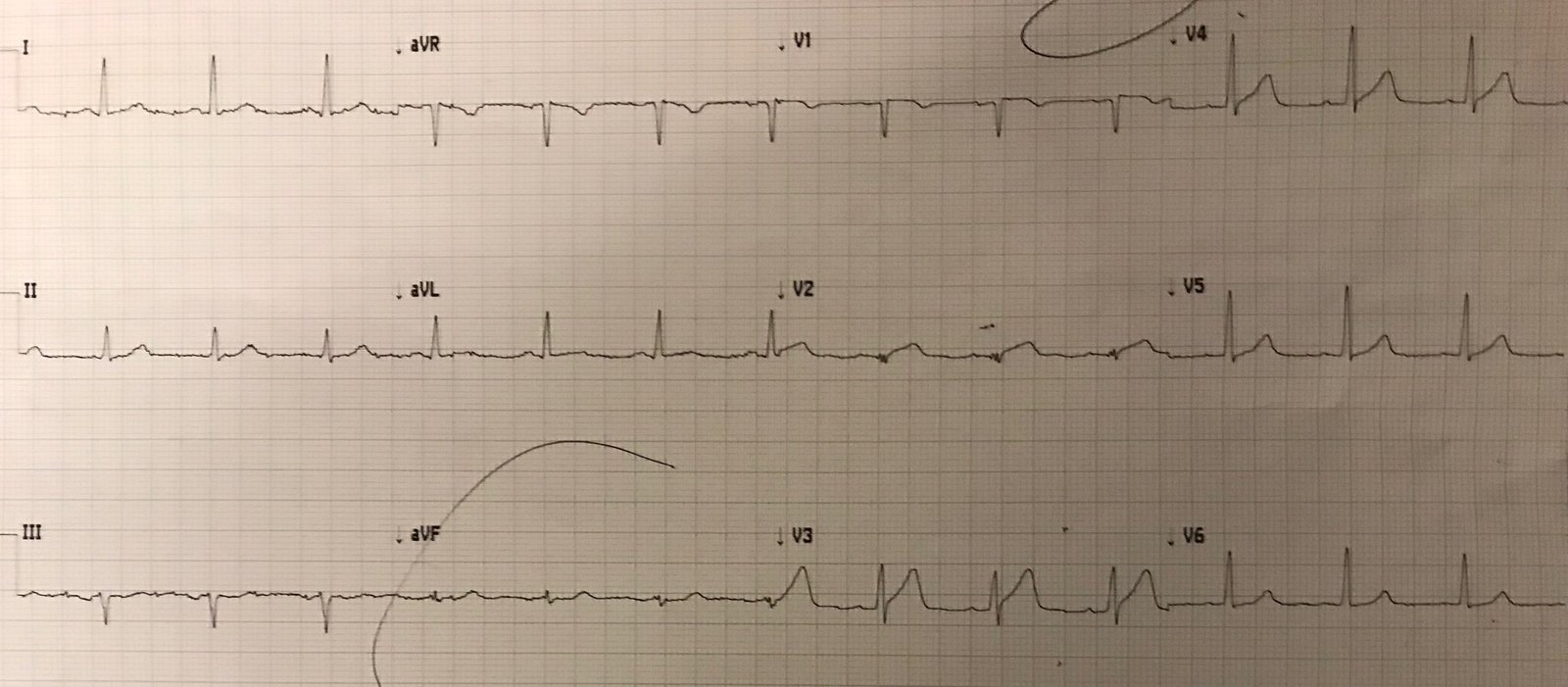
So a bedside echo was done:

Large effusion.
Diagnosis: Pericarditis.
= = =
======================================
MY Comment, by KEN GRAUER, MD (1/22/2026):
Today’s case by Dr. Smith is quick but important. It highlights the following: i) The importance of the history; — ii) ECG findings of acute pericarditis vs acute OMI; — and, iii) A refresher on What does vs What does not constitute T-QRS-D (Terminal-QRS–Distortion). I focus on these 3 issues in My Comment below.
= = =
The History is Everything!
As is frequently emphasized on Dr. Smith’s ECG Blog — Among patients without potential predisposing conditions, who present for emergency care because of new-onset CP (Chest Pain) — the diagnosis of acute pericarditis is rare.
- The above said — Today’s patient does have potential “predisposing” conditions. These are: i) Esophageal cancer; — and, ii) Pleural effusion on Chest X-Ray, thereby suggesting there may be cancer spread to neighboring areas. As a result, statistical likelihood of pericarditis is significantly increased.
- Today’s patient does not have CP! This greatly reduces statistical likelihood for this patient to have an ongoing exensive acute STEMI (as would be the case if the diffuse ST elevation seen on his ECG was the result of acute coronary occlusion).
- BOTTOM Line: Although I have fully adopted Dr. Smith’s mantra (ie, that you diagnose acute pericarditis at your peril! ) — these words of caution do not hold true in today’s case because of the presence of predisposing conditions for pericarditis — and because of the absence of chest pain. Thus, the history tells us (even before looking at today’s ECG) — that there is a reasonable chance this patient may have acute pericarditis.
= = =
ECG Findings for and against Acute Pericarditis …
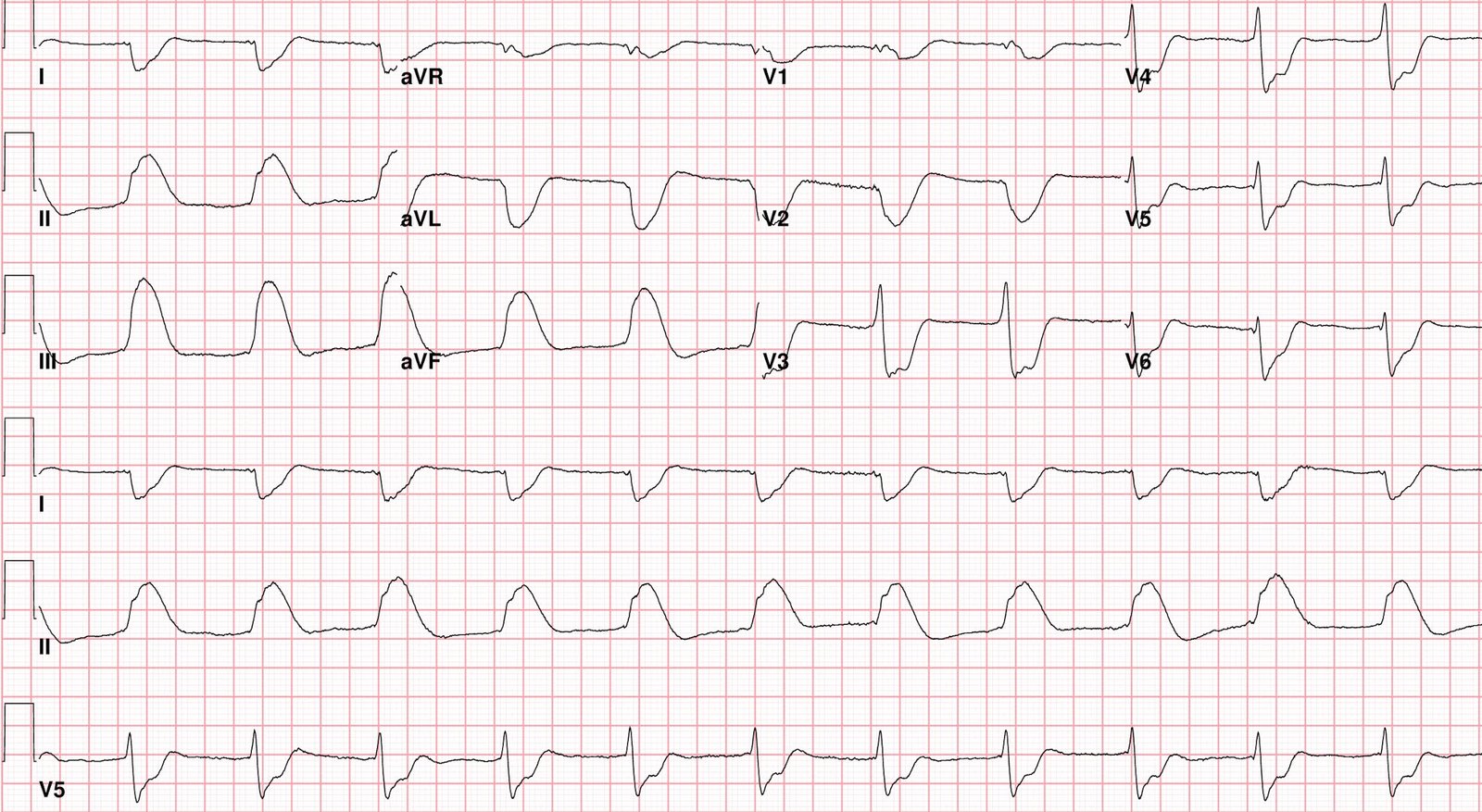
For clarity in Figure-1 — I’ve reproduced and labeled today’s ECG.
- Note in Figure-1 that there is diffuse ST elevation. This is present in no less than 9/12 leads, which is consistent with acute pericarditis (acute OMIs more commonly localize ST elevation — and generally do not manifest ST elevation in so many leads).
- The shape of this ST elevation in Figure-1 is concave up (ie, “smiley” configuration) — which is typical for acute pericarditis (acute OMIs more commonly manifest a coved or convex down = “frowny” configuration)
- There is essentially no reciprocal ST depression (as would especially be expected in the inferior leads given the amount of chest lead ST elevation that is already marked as early as in lead V2).
- Additional findings in favor of acute pericarditis include: i) PR depression in a number of leads, with PR elevation in lead aVR; — ii) There is normal R wave progression (whereas with acute anterior MI — there is often delayed transition with loss of R wave amplitude in the anterior leads); — iii) ST-T wave in lead II resembles that seen in lead I more than that seen in lead III; — and, iv) The ST/T wave ratio appears to be greater than 0.25 (See My Comment at the bottom of the page in the September 28, 2025 post for “My Take” on ECG findings in acute pericarditis).
- BOTTOM Line: In association with the history in today’s case — the ECG in Figure-1 is clearly more suggestive of acute pericarditis than acute MI. That said — even proximal LAD occlusion may not always manifest reciprocal changes in the inferior leads — and ST elevation in 9/12 leads can be seen with an extensive acute STEMI. As a result (like Dr. Smith) — I was not prepared to write off the possibility of acute LAD occlusion on the sole basis of the initial ECG.
= = =
Figure-1: I’ve labeled today’s ECG.
= = =
In Figure-1 — Is there T-QRS-D?
We often highlight the importance of recognizing T-QRS-D — since IF this unique ECG finding is present — it essentially rules out repolarization variants and rules out acute pericarditis — and — it essentially rules in acute OMI (For illustration and review of T-QRS-D — Check out My Comment at the bottom of the page in the May 8, 2025 and January 19, 2026 posts).
- T-QRS-D — is defined as the absence of both a J-wave and an S-wave in either lead V2 or lead V3 (and probably also in lead V4). Although simple to define — this finding may be subtle!
- A J-wave may manifest as either a notching or slurring that occurs where the end of the QRS joins the beginning of the ST segment (ie, the J-point joins the S of the QRS to the beginning of the ST segment).
To Emphasize: T-QRS-D is not a common finding with acute OMIs. But because of the diagnostic specificity of T-QRS-D if it is found — I carefully considered leads V3 and V4 in Figure-1 for the possibility of this finding.
- In lead V4 — there is no S wave (ie, The terminal end of the R wave downslope does not reach the baseline — therefore there is no S wave in this lead). But because there is a prominent notch (highlighted by the YELLOW arrow in lead V4) — this is not T-QRS-D.
- In lead V3 — the J wave is much more subtle (ie, I had to look closely at the magnified insert of this lead to appreciate that a subtle J-point notch is present in lead V3). That said — the S wave in V3 easily reaches the baseline — so T-QRS-D is not present.
= = =
CASE Conclusion:
- Dr. Smith’s approach quickly resolved this case. Starting from the likelihood of acute pericarditis (based on predisposing conditions — the absence of CP — and an ECG with a series of findings in favor of acute pericarditis) — quick performance of bedside Echo showing a large pericardial effusion was all that was needed to provide the needed confirmation.
= = =
= = =