A 50-something male with h/o CAD and CABG, and dual chamber pacemaker due to sick sinus syndrome, called 911 for onset of acute chest pain 2 hours prior.
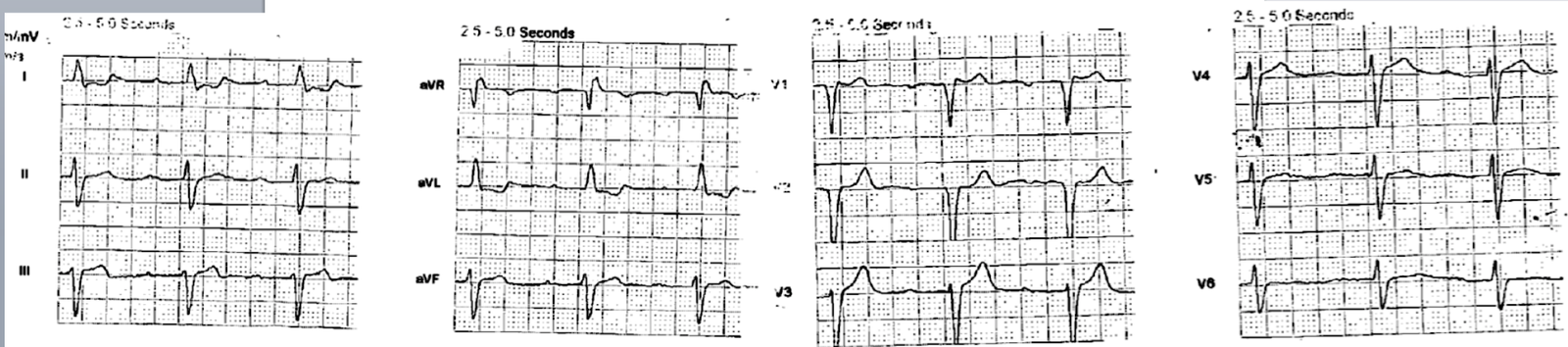
Here was the prehospital ECG:
The medics brought the patient to the critical care area, as they were suspicious of acute MI.
The pain started at rest, was constant, sharp in the sternum and radiating to the jaw and left arm and into the upper back, associated with diaphoresis but no SOB. No history of venous thromboembolism. It was not relieved with nitroglycerin at home, but decreases from 9/10 to 7/10 after EMS gave NTG. He stated it felt like a prior MI.
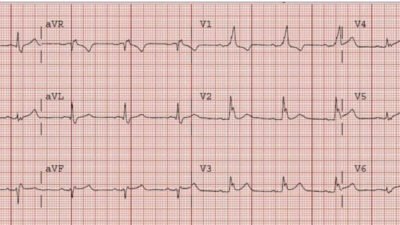
Here is the first ED ECG, at time zero:
The prehospital ECG has normal conduction without ischemic ST elevation.
The ED ECG now has a ventricular paced rhythm (VPR).
The ED ECG now has new ST Elevation.
Is all this new ST elevation only due to VPR.
No!
Smith modified Sgarbossa criteria (for use in LBBB and in VPR):
Rule 1 (80-90% sensitive, 95% specific)
Any one of:
1. 1 mm concordant STE in any one lead.
2. 1 mm concordant STD in any one of leads V1-V3
3. At least 1 mm discordant STE that is greater than or equal to 25% of preceding S-wave in at least one lead.
Rule 2 (Only 64% sensitive, but 98% specific, for occlusion):
Any single lead with proportionally excessively discordant STE or STD of at least 30% of preceding S- or R-wave.
Lead aVL seems to have STD that is at least 30% of preceding R-wave.
Smith modified Sgarbossa criteria are being studied now in the PERFECT study (Paced ECG Requiring Fast Emergent Coronary Therapy). Preliminary Results are encouraging that they work in ventricular paced rhythm as well (not surprisingly). See abstract and references below.
___________________
Case continued
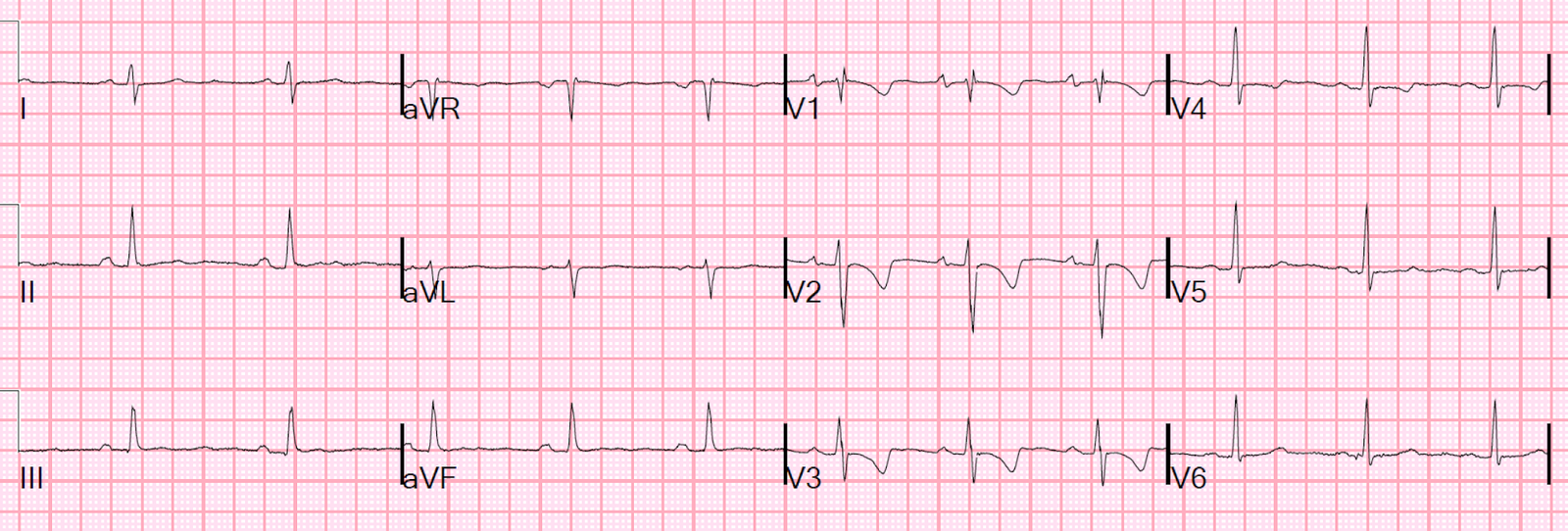
The physicians were worried about this, and 16 minutes later recorded this ECG:
 |
| Now there is clearly excessively discordant STE in III and aVF, with excessive STD in aVL. Notice there is also quite a bit of ST elevation in V1; is this due to RV MI? |
The cath lab was activated.
It was a very interesting angiogram.
There was a known chronically occluded proximal RCA, proximal to the RV marginal branch supplying the RV.
The RCA distal to this was known to be supplied by a CABG graft to the posterolateral branch of the RCA (on the posterior wall!), such that flow to the RCA was retrograde.
This posterolateral branch (not the graft itself) was occluded such that that branch could no longer supply the inferior wall and the RV.
Therefore, it caused inferior and RV STEMI.
It was opened and stented with good results.
Full angiogram report:
1. Left main: patent stent.
2. LAD: 70% stenosis in the mid segment at the take-off of a diminutive D1 (angiographically unchanged from previous angiography in 9/2017), then >90% stenosis after D2 (D2 has a 2.0-2.5 mm caliber). The distal LAD is supplied by a patent LIMA.
3. LCX: chronically occluded. The OM is supplied by a patent vein graft.
4. RCA: known chronic occlusion, therefore not studied. The RPLA is supplied by a patent vein graft. Antegrade flow into the RPLA is good, however, retrogradely the RPLA is occluded with contrast hang-up indicative of a thrombotic occlusion. Hence the flow to the RPDA is compromised.
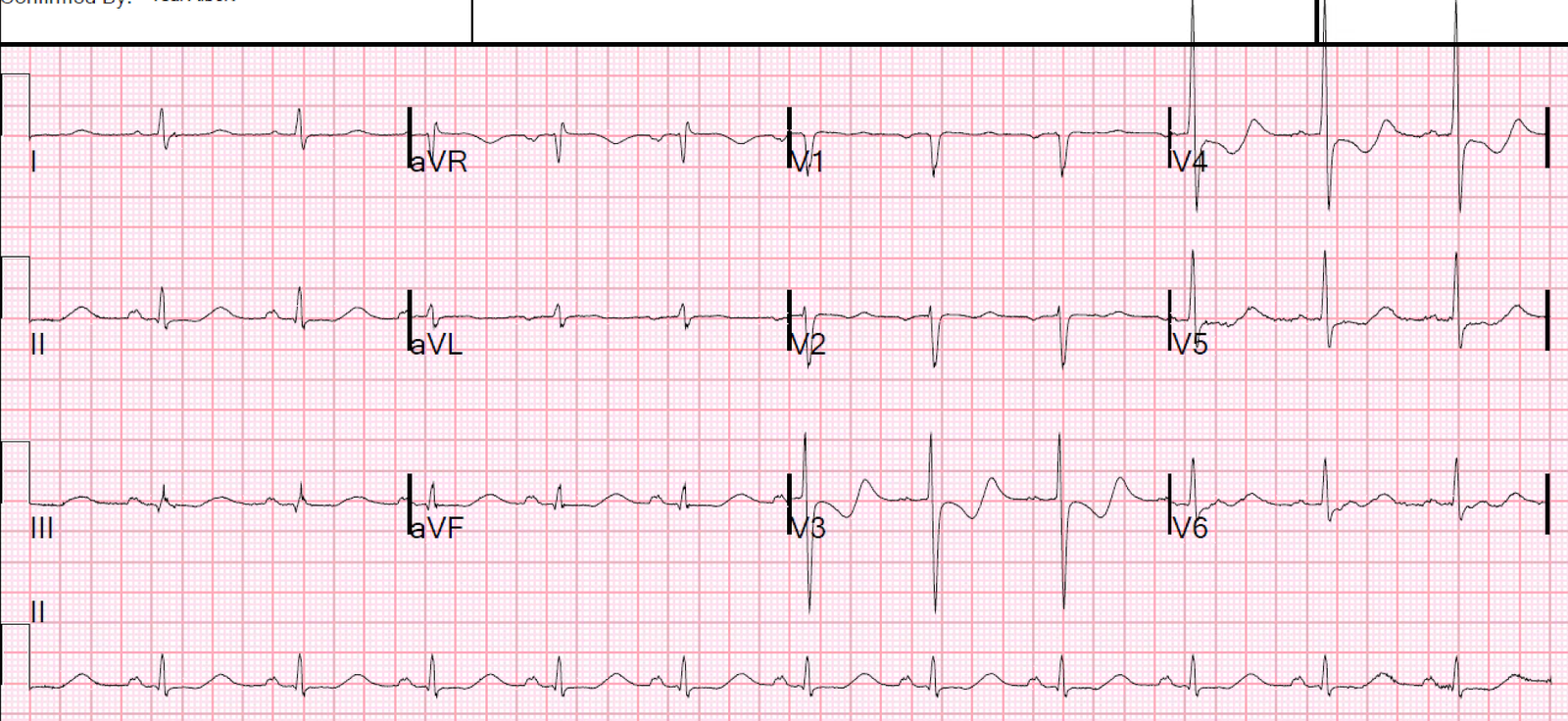
Here is the post intervention ECG:
The patient went into a paced rhythm, and so had a paced ECG recorded about the same time post cath as the above ECG:
Peak troponin = 8.2 ng/mL
Echo:
The estimated left ventricular ejection fraction is 50 %.
Regional wall motion abnormality-basal inferior, hypokinetic.
Learning Point:
Modified Sgarbossa Criteria are very useful in Ventricular Paced Rhythm
Smith modified Sgarbossa criteria:
–>