An elderly woman called 911 for SOB. She had a history of COPD. On arrival, she was cyanotic and had increased work of breathing. En route to the hospital, she had a bradycardic arrest.
She had ROSC, and a Bedside echo showed a large RV and very small LV. The providers made a provisional diagnosis of pulmonary embolism based on this clinical presentation.
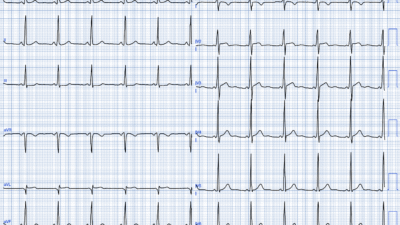
Here is the first ECG:

What do you think?
There is atrial fibrillation. There is RBBB with right axis deviation (deep S-wave in I, with R/S ratio < 1), including a probable left posterior fascicular block. The R-wave amplitude in right precordial leads is very large. I saw this on the EKG system before I ever knew about the case and thought that this was likely right ventricular hypertrophy (RVH)
Continue:
She arrested again and was given tPA for presumed pulmonary embolism. She was also put on ECMO.
She had another ECG recorded:

The RBBB is no longer present, as the QRS duration is less than 120 ms. More importantly, the R’-wave in V1 is not at all wide. But it does have a lot of amplitude! The right axis deviation is again present (deep S-wave in lead I), and it cannot be blamed on RBBB. There is a large R-wave in V1; R/S ratio is > 1. This is diagnostic of RVH (right ventricular hypertrophy).
There is also of course much diffuse ST depression, diagnostic of diffuse subenocardial ischemia, which is typical of a post-ROSC heart.
A CT scan was done and did not show pulmonary embolism.
Troponin I rose to greater than 60,000 ng/L. Angiogram was negative.
Formal echo showed severe RV hypertrophy.
The providers never recognized the ECG findings, which are very specific for RVH.
Recognizing RVH probably would not have changed the management of this patient, since there could be superimposed pulmonary embolism. But, in many cases, it is very helpful to recognize RVH. This patient has COPD, which causes cor pulmonale and pulmonary hypertension. People with RVH are at extremely high risk of cardiac arrest especially when hypoxic or hypotensive. The arrest is completely compatible with RVH + severe COPD exacerbation. Knowing that could have an effect on the decision to give thrombolytics.
RVH is rarely recognized on the ECG. The ECG is VERY useful for the differentiatial diagnosis of a large RV on bedside ultrasound, between PE and RVH, as PE shows only acute right heart strain, and RVH has a large R-wave in V1. (V1 is placed directly over the RV; it is only enlarged with chronic RVH, not with acute right heart strain).
I once watched a lecture by one of the nation’s experts in RV Failure, Susan Wilcox. She presented a number of cases of RV Failure that went undiagnosed. In every case for which she showed the ECG (as I remember, it was 4 cases), the ECG showed RVH, but Dr. Wilcox had not been aware of it. I contacted her about this in order to call her attention to it, and she had indeed not been aware of it. She was very gracious and appreciative to learn about it.
See these other cases of RVH:
What does the ECG show in this patient with chest pain, hypotension, dyspnea, and hypoxemia?
Dyspnea and chest pain. O2 saturation 88%.
An elderly woman with shortness of breath and an ECG that helps understand it
21 year old woman with CP, SOB, then syncope, and with ST depression with T-wave inversion in V1-V3
ST Depression and T-wave inversion in V2 and V3.
A 50-something male with Dyspnea
This was texted to me by a former resident. An 80-something woman who presented with chest pain and dyspnea.
What is going on in V2 and V3, with a troponin I rising to 1826 ng/L at 4 hours?
55 year old woman with chest pain and precordial T-wave Inversions
======================================
MY Comment, by KEN GRAUER, MD (1/4/2026):
Today’s case highlights this point by Dr. Smith:
- The ECG diagnosis of RVH is often difficult to make — and simply not thought of. As a result — it gets overlooked, which all-too-often has unfortunate clinical implications.
= = =
RVH is Often Overlooked …
I’ve reviewed “My Take” on why the ECG diagnosis of RVH is so often overlooked on a number of occasions (See the February 12, 2023 post) — not the least of which are:
- i) That our “medical eye” is used to looking for LVH, which in adults is so much more common than RVH; — and,
- ii) In order for the anatomically smaller and much thinner RV to become hypertrophied enough in an adult to sufficiently overcome the predominance of LV electrical forces — RVH with cor pulmonale will usually have progressed to a very advanced stage (which is very different than the process for developing RVH in young children with congenital heart disease — in whom RVH is a common finding that is much more easily apparent on ECG).
= = =
RVH Diagnosis is Complicated by RBBB …
The ECG diagnosis of RVH becomes even more challenging in the presence of complete RBBB (Right Bundle Branch Block). This is because the criterion of a predominant R wave in lead V1 is electrically counterbalanced by the conduction defect of RBBB, in which an anatomically much smaller RV may produce a deceptively tall ECG waveform (ie, R wave in lead V1) when the RV is left depolarizing by itself after LV depolarization has finished (which is what occurs with RBBB).
- The ECG criterion that I have most commonly seen cited for diagnosis of RVH when there is also complete RBBB — is an R’ in lead V1 ≥10-15 mm. In my experience over a period of decades, of looking for RVH in association with RBBB (using Echo correlation as my “gold” standard) — this R’ amplitude criterion in lead V1 is associated with a considerable number of false positives and false negatives.
- Looking for RVH on ECG in patients with incomplete RBBB (which I define as an rbbb pattern with a QRS duration of <0.11 second) — is easier, because significant increased amplitude for the R’ wave in lead V1 (ie, greater than 5-10 mm) — is more specific for RVH when there is incomplete RBBB, because the RV is not depolarizing unopposed by LV forces to nearly the same extent as it is when there is complete RBBB.
- The presence of RAD (Right Axis Deviation), in which there is a predominant S wave in lead I — is much more supportive of true RVH in association with incomplete RBBB than it is with complete RBBB (Simply stated — a wide terminal S wave in lead I is expected as an essential part of RBBB criteria — because this finding primarily reflects terminal unopposed RV depolarization and not RV size).
= = =
Application to Today’s ECGs …
With the above as background — I found assessment of today’s 2 ECGs to be fascinating. For clarity and ease of comparison — I’ve reproduced and labeled these 2 tracings in Figure-1.
- As per Dr. Smith — the rhythm in ECG #1 is relatively rapid and irregularly irregular without P waves = AFib with a somewhat increased ventricular response (average rate a bit over ~110/minute).
- Complete RBBB is diagnosed in ECG #1 by the widened ( = 0.12 second in this tracing) QRS duration with predominant R wave in lead V1 + wide terminal S wave in lateral lead I (this S wave in lead I not being deep enough to qualify for LPHB).
- The presence of AFib negates our potential use of finding RAA as a supportive criterion for RVH (For review of my approach to the ECG diagnosis of RAA, as well as LAA — CLICK HERE).
- However — in the setting of RBBB, the loss of the initial positive r wave deflection, to form a qR pattern in Lead V1 suggests there is pulmonary hypertension! (See my Figure-2 in My Comment at the bottom of the page in the February 12, 2023 post for illustrated discussion of why this is so).
- I thought the tiny, multiphasic QRS complex in lead V2 looked “out-of-place” in the context of the appearance of the remaining chest leads in ECG #1 (most probably the result of inaccurate lead placement — be this due to the patient’s female gender or advanced COPD anatomy).
- R wave amplitude is huge in lead V3 — and certainly could reflect marked RVH (although I’m unaware of any ECG criteria for RVH that are based on R wave amplitude in lead V3).
- Finally — I interpreted the diffuse and marked ST-T wave depression that is maximal in the inferior and anterior leads, as potentially consistent with RV “strain” (albeit difficult to distinguish RV “strain” from the effect that new, fairly fast AFib might have on ST-T waves).
BOTTOM Line: RVH in an adult is a difficult diagnosis to make based solely on ECG. It is especially difficult to diagnose in association with complete RBBB (and especially when there most probably is an error in chest lead placement).
- The above said — this patient’s known history of COPD, now with acute dyspnea, cyanosis and bradycardic arrest clearly predisposes her to RVH — especially with the ECG finding of a qR pattern in V1 ( = the above observations all supportive of the clinical concept that RVH on ECG is a “detective diagnosis” — not to be made based on any single ECG finding — but rather dependent on clinical context in association with all ECG findings found on the tracing).
- I thought ECG #1 could clearly be consistent with acute PE — as new AFib is a not uncommon arrhythmia in this situation, especially in a longterm COPD patient predisposed to preexisting RVH.
- Bedside Echo quickly confirmed the ECG impression of RVH (albeit with a very small LV). Subsequent chest CT confirmed there was no acute PE.
= = =
Figure-1: I’ve reproduced and labeled the 2 ECGs in today’s case.

= = =
Today’s Repeat ECG …
The repeat ECG in today’s case was obtained following ROSC after a 2nd cardiopulmonary arrest (with ECG #2 recorded after this patient was placed on ECMO). Other clinical details are not temporally correlated — leaving us to wonder about reasons for some of the marked differences between ECG #2 vs ECG #1.
- Sinus rhythm has been restored in ECG #2. Although the upright P wave in lead II does not satisfy the ≥2.5 mm amplitude voltage criteria for RAA (Right Atrial Abnormality) — the distinctly pointed shape of the upright P wave in leads II,III and aVF still strongly suggests RAA given the clinical context.
- The QRS is no longer wide in ECG #2 (I measure 0.10 second in duration). There is now a distinct triphasic (rSR’) pattern in lead V1 — with terminal (albeit narrow) S waves in lateral leads I and V6 ==> therefore consistent with incomplete RBBB.
- In the context of a normal duration QRS complex — the predominantly negative QRS in lead I clearly indicates RAD (Right Axis Deviation).
- There once again is strong suggestion of lead misplacement for lead V2 — with the small amplitude rS pattern in this lead not making sense to me given the triphasic rbbb-like appearance in both of its neighboring leads ( = leads V1 and V3).
BOTTOM Line: Looking at ECG #2 alone — I’d interpret this tracing as sinus rhythm + RVH (given the clinical context of known severe pulmonary disease with the findings of IRBBB, RAD, and RAA on ECG). Once again — R’ amplitude in lead V3 is huge (albeit significance of this finding is uncertain).
- I’d be intellectually curious as to why the QRS so suddenly became narrow — especially with loss of the qR pattern in lead V1 (? marked improvement in hemodynamics on ECMO that was started after the 2nd cardiopulmonary arrest?).
- Finally — the QTc is now markedly prolonged in ECG #2, seen here in association with dramatic diffuse ST depression. Whether this reflects post-resuscitation ischemia or CNS insult following a 2nd cardiopulmonary arrest is uncertain.
- Hopefully the patient went on to recover …
= = =
= = =