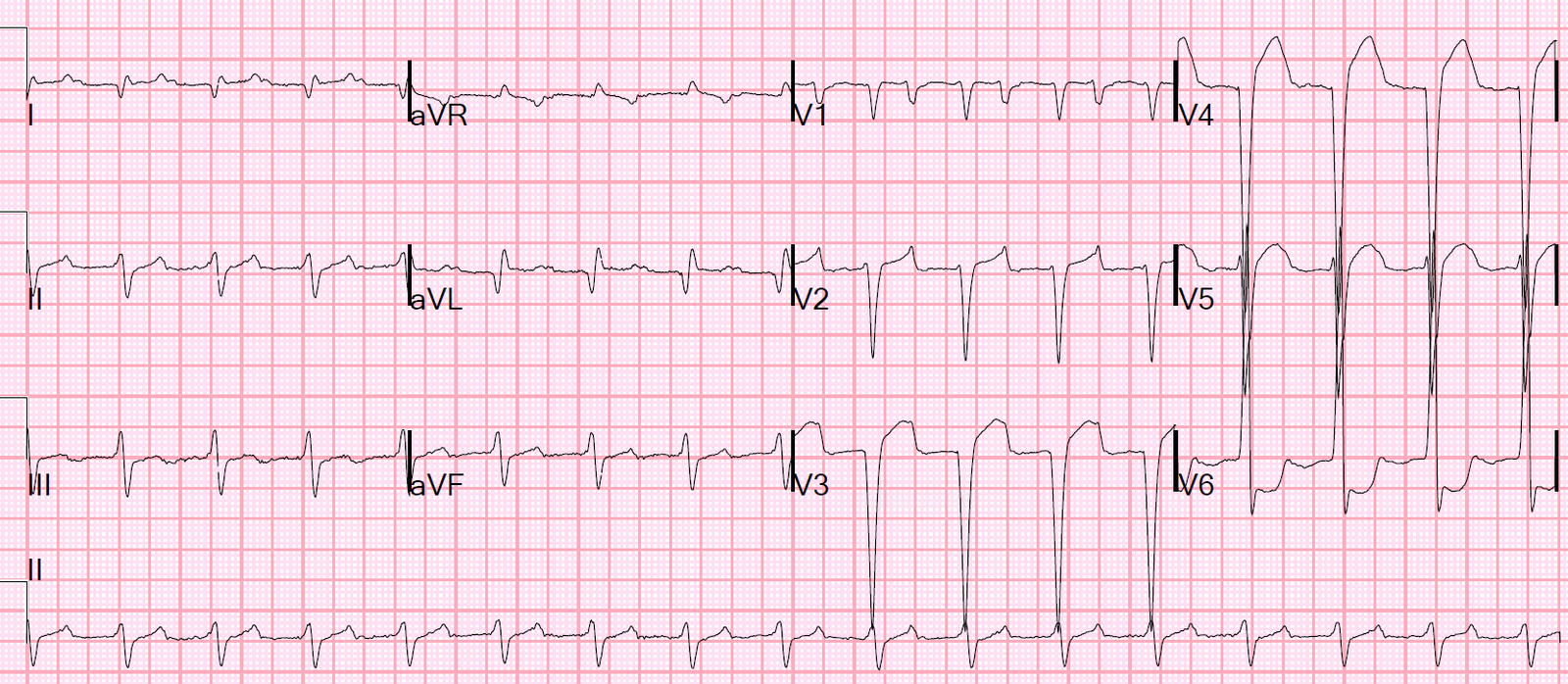
This patient has a history of cardiomyopathy (EF 10%) and IVCD and heart failure and presented with altered mental status. BP was 87/52, pulse 90, saturations 100%, and respirations 14. An ECG was recorded:
There was an ECG from 4 months prior:
 |
| Atrial fib. QRS = 118 ms. Voltage was high then too, but ST segments were not. So the ST elevation is new. |
The physicians were worried about this and showed it to me.
I said that this is very unlikely to be ischemia because of:
1) the severe cardiomyopathy
2) the high voltage
3) relative clinical stability in a patient with a baseline EF of 10%
4) presentation without chest pain
I recommended a bedside echo and further eval. This was done and showed very poor LVF and no WMA.
Electrolytes and Venous Gas results returned:
Na = 117 mEq/L
K = 2.7 mEq/L
Chloride = 68 mEq/L (this indicates metabolic alkalosis)
CO2 = 46 mEq/L
Anion Gap = 3 mEq/L (so there is no serious metabolic acidosis)
Venous pH = 7.58 (normal = 7.33), corresponds to an arterial pH of 7.65 (very alkalemic)
HCO3 = 45
Venous pCO2 = 47 (normal = 47), which corresponds to an arterial pCO2 of about 40 mmHg.
This actually represents a superimposed respiratory alkalosis: when the HCO3 = 45, the patient should compensate with a decrease in minute ventilation, such that the arterial pCO2 should be about 57 (0.9 x HCO3 + 15), and venous pCO2 should be slightly higher, around 62-64 mmHg, not 47 mmHg.
For a comprehensive presentation on Acid Base disturbances, see my 55 minute lecture on the topic.
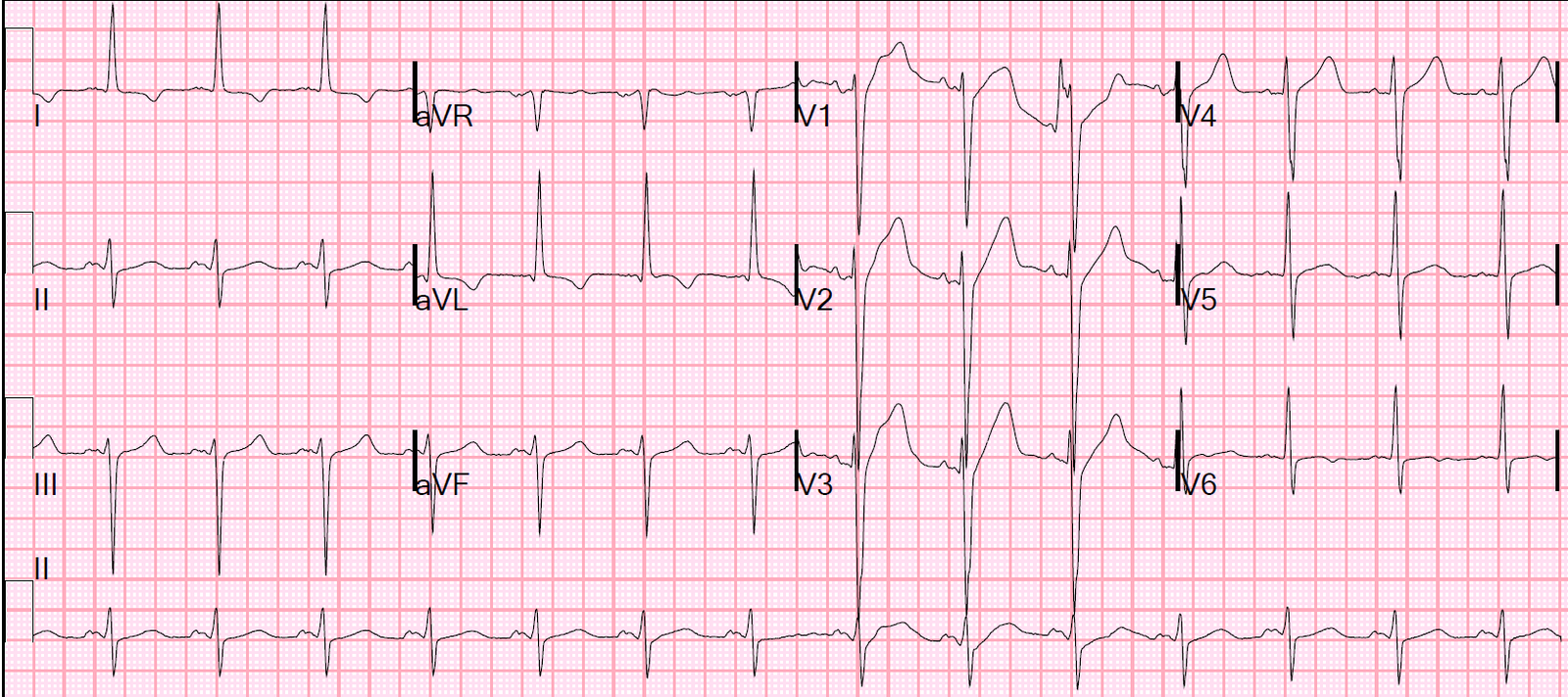
So the patient has profound metabolic disturbances [hypokalemic metabolic alkalosis without any respiratory compensation (and thus a superimposed resp alkalosis)], and this explains the ECG findings. After some treatment, this ECG was recorded 23 hours after the first:
 |
| It is normalizing |
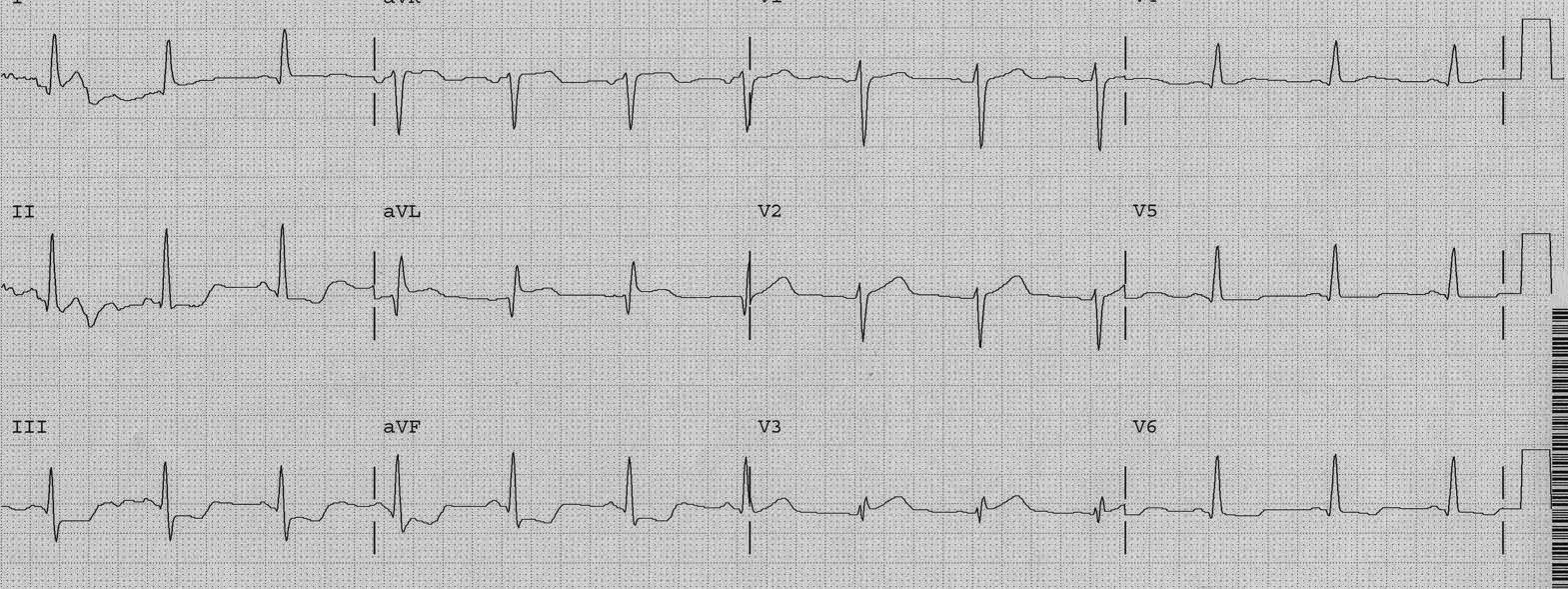
At 36 hours, after more electrolyte correction:
 |
| Looking more and more like the old ECG |
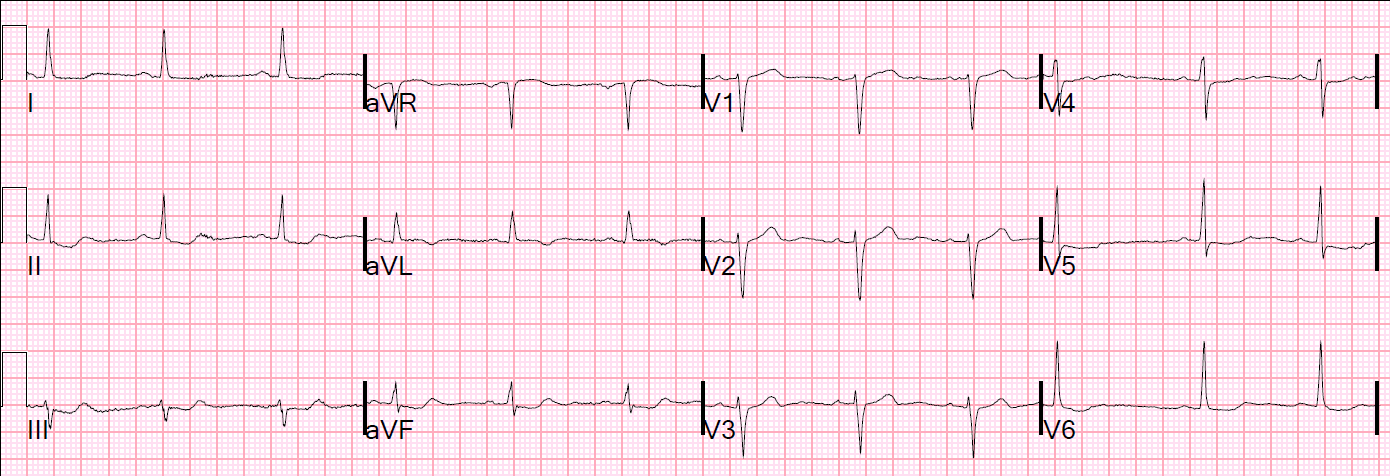
At 3.5 days, there was some tachycardia:
 |
| This was diagnosed as SVT, but it is, in reality, sinus tachycardia. See image below with arrows. |
Annotated
 |
| Arrows point to P-waves. Note the P-wave morphology, and PR interval, are the same as in the slower sinus rhythms. |
Learning Points:
Cardiomyopathy, especially with metabolic derangement, can result in profound PseudoSTEMI patterns.