Written by Alex Bracey with edits from Pendell Meyers and Steve Smith
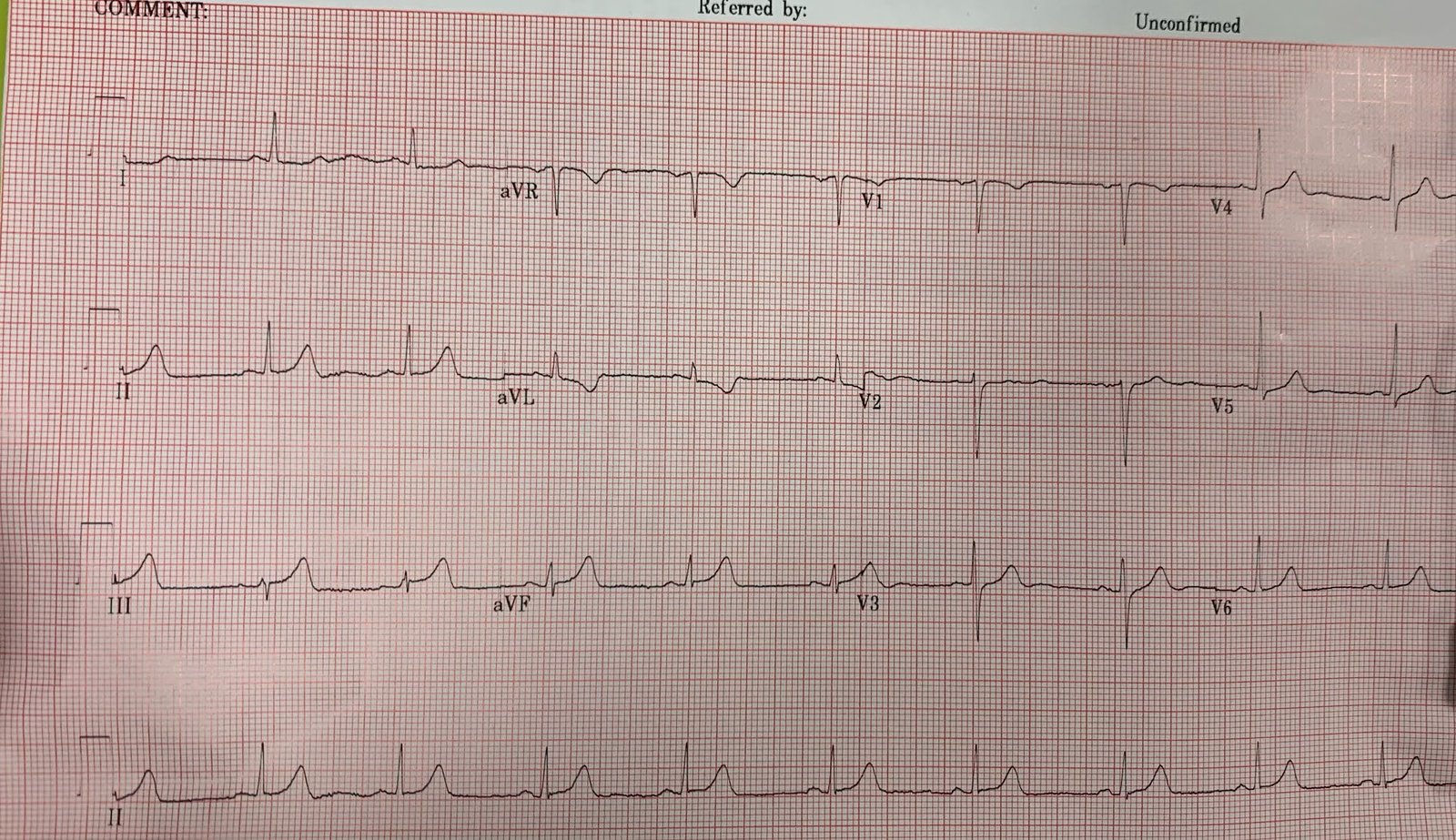
A woman in her 60s presented to the ED as a referral from an urgent care for weakness. When I interviewed her, she reported that she had experienced several months of shortness of breath and fatigue, which had worsened in the last several days. She had also experienced new dyspnea on exertion, along with a non-productive cough and fatigue. The only medical problem she was aware of was hypertension treated with hydrochlorothiazide. An ECG was performed as follows:
 |
| Sinus tachycardia Convex, upward ST elevation in V1-V4 with subsequent T wave inversion Right axis deviation |
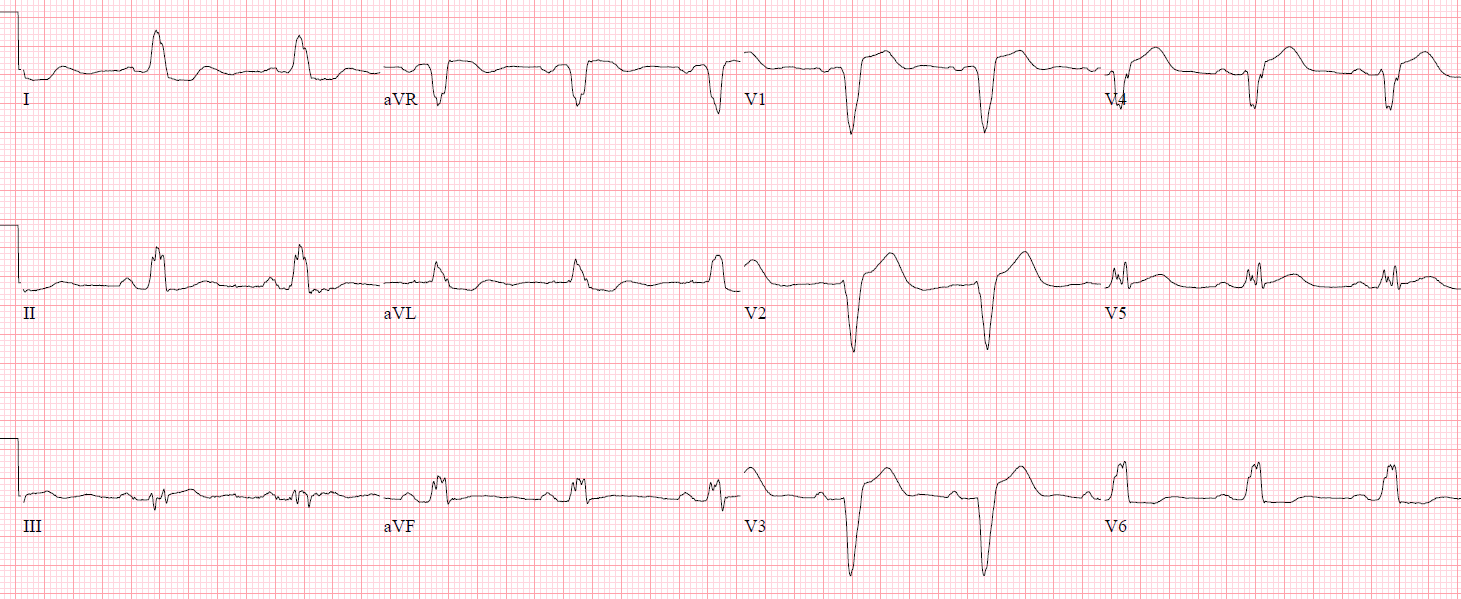
Based on this ECG, I was concerned about right heart strain, including pulmonary embolism (PE); however, this ECG could be seen in any condition that causes right heart strain, both acute and chronic. Her story did not neatly fit into any one diagnosis. Typically, my practice is to use a risk-stratification tool (e.g., Wells’ Criteria for PE, modified Geneva) to help guide my diagnostic testing in the evaluation of PE. Importantly, ECG is not used in these commonly utilized tools. Despite an HPI and an exam that did not suggest PE as a clear diagnosis, I ordered a CT angiography of the pulmonary arteries while my resident performed a bedside cardiac ultrasound:
Imperfect parasternal short axis view
Right ventricle is clearly greater than one-third the size of the left ventricle (nearly equal)
Septal flattening with probable septal bowing (D-sign)
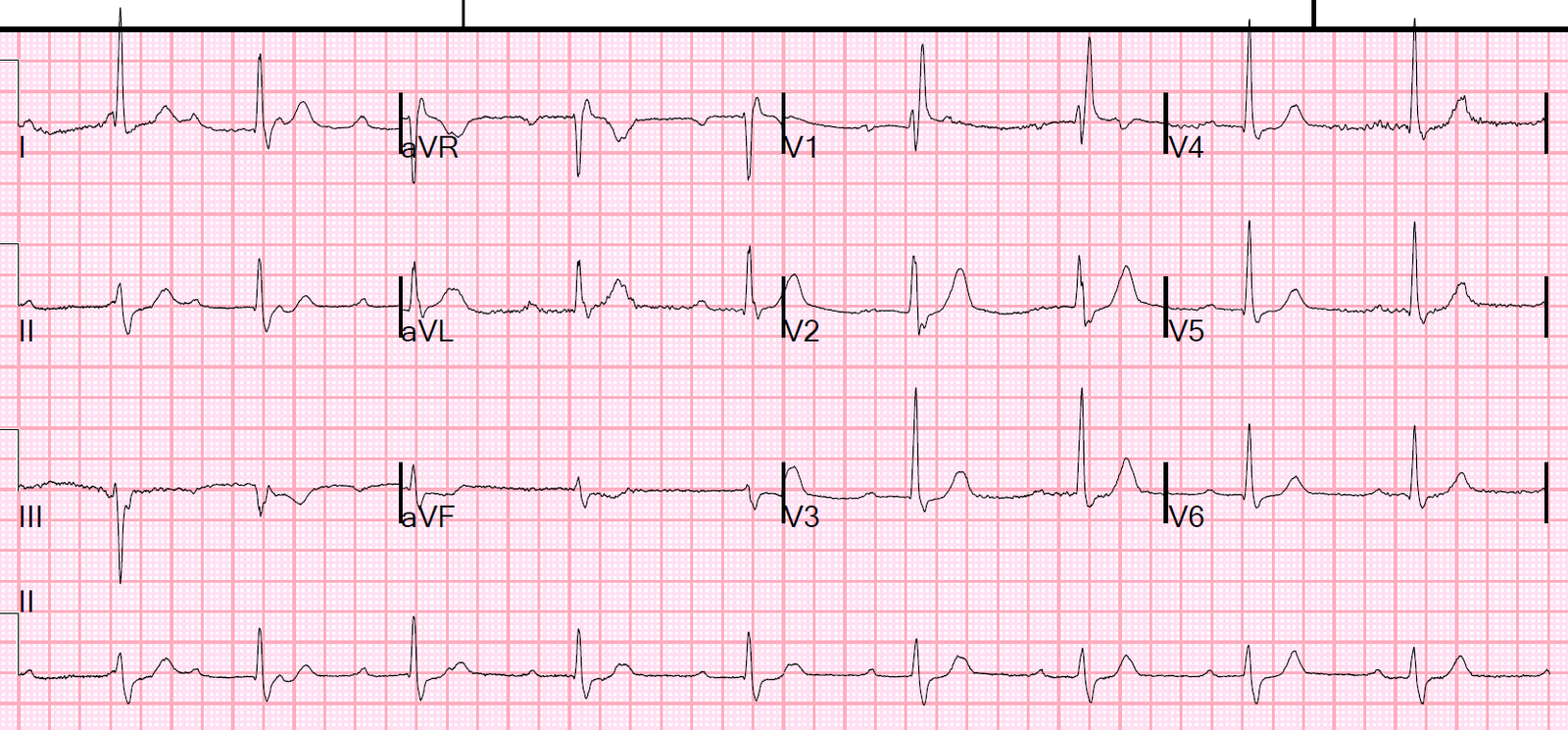
Initial troponin I was undetectably low (negative), BNP was elevated to 582 pg/mL (reference values 0 – 100) and lactic acid was elevated to 2.2 mmol/L. A D-dimer ordered from triage resulted at 3.30 (Reference: <0.50 mg/L). Shortly afterwards, the patient underwent CTPA:
 |
| CT angiography of the pulmonary arteries in the axial view demonstrating bilateral, central pulmonary emboli |
The patient was started on anticoagulant therapy and had an uncomplicated hospital course.
Teaching points:
– Patients often have presentations that are not “classic” for a given disease. Paying attention to clues from ancillary testing may help to better diagnose, and ultimately to care for our patients. The subtle findings on this ECG helped to expediently come to the correct diagnosis in this case.
– ECG findings are not used in many commonly used risk-stratification tools for PE. In this case, had PE been considered as a diagnosis based on history and a risk-stratification tool subsequently been applied, testing with D-dimer would have been indicated and have had a positive result. Therefore, a CTPA would have been performed and the PE discovered. However, the ECG may heighten concern and expedite care, such as in this case.
– The ECG findings in this case can be caused by process causing right heart strain, in this case pulmonary embolism was the culprit.
Other cases of right heart strain and pulmonary embolism on the blog:
A crashing patient with an abnormal ECG that you must recognize
A man in his 40s with a highly specific ECG
Chest pain, ST Elevation, and tachycardia in a 40-something woman
Repost: Syncope, Shock, AV block, RBBB, Large RV, “Anterior” ST Elevation in V1-V3
A young woman with altered mental status and hypotension
An elderly woman transferred to you for chest pain, shortness of breath, and positive troponin – does she need the cath lab now?
A crashing patient with an abnormal ECG that you must recognize
A 30-something woman with chest pain and h/o pulmonary hypertension due to chronic pulmonary emboli
A 30-something with 8 hours of chest pain and an elevated troponin
Syncope, Shock, AV block, Large RV, “Anterior” ST Elevation….
Dyspnea, Chest pain, Tachypneic, Ill appearing: Bedside Cardiac Echo gives the Diagnosis
31 Year Old Male with RUQ Pain and a History of Pericarditis. Submitted by a Med Student, with Great Commentary on Bias!
Chest pain, SOB, Precordial T-wave inversions, and positive troponin. What is the Diagnosis?
Cardiac Ultrasound may be a surprisingly easy way to help make the diagnosis
Answer: pulmonary embolism. Now another, with ultrasound….
This is a quiz. The ECG is nearly pathognomonic. Answer at bottom.
Chest Pain, SOB, anterior T-wave inversion, positive troponin
Anterior T wave inversion due to Pulmonary Embolism