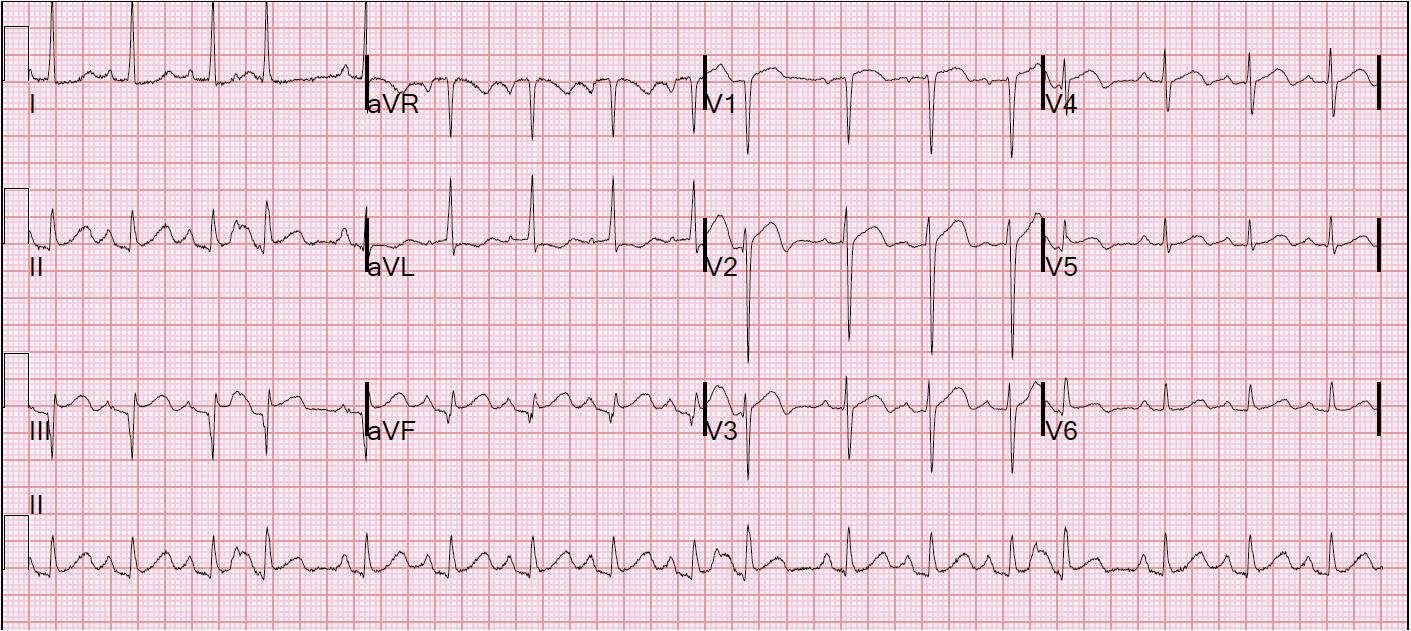
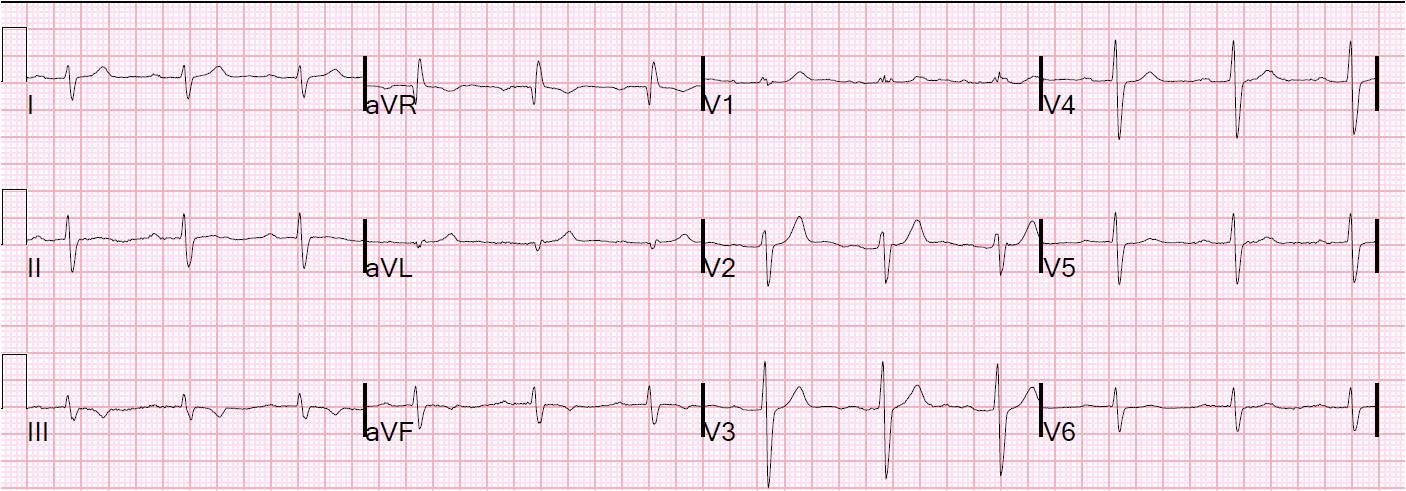
This is a 58 year old woman with a history of inferior MI. She has had a week of intermittent substernal chest heaviness associated with SOB. Because it came again and lasted for one hour, she called 911. The medics recorded a 12-lead, then gave her aspirin and nitro, and her pain resolved completely. It seems the physicians caring for her did not see this ECG, so I am not showing it first. On arrival in the ED around midnight, she was pain free and had this ECG recorded:
The first ECG is substantially different from the previous ECG 3 years prior:
 |
| Previous ECG from 3 years prior shows old inferior MI and baseline precordial ST elevation of early repolarization. There is upward concavity and normally upright T-waves. |
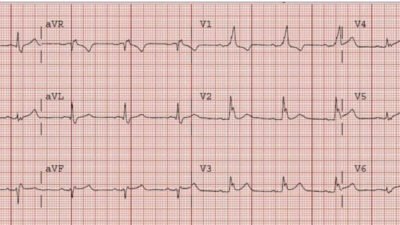
Prehospital ECG during chest pain, before nitro and aspirin.
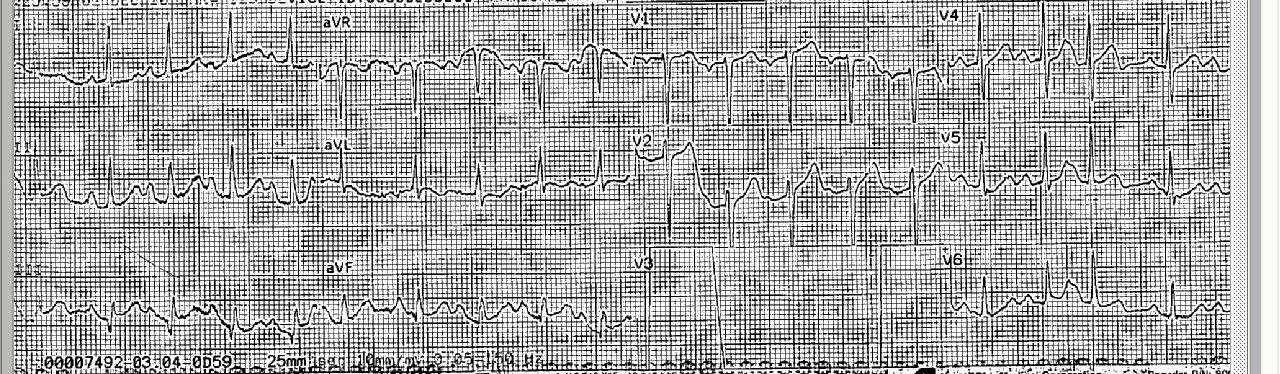 |
| There is ST elevation and a large upright T-wave in V1, different from the baseline T-wave. The LAD may well have been occluded during this recording. |
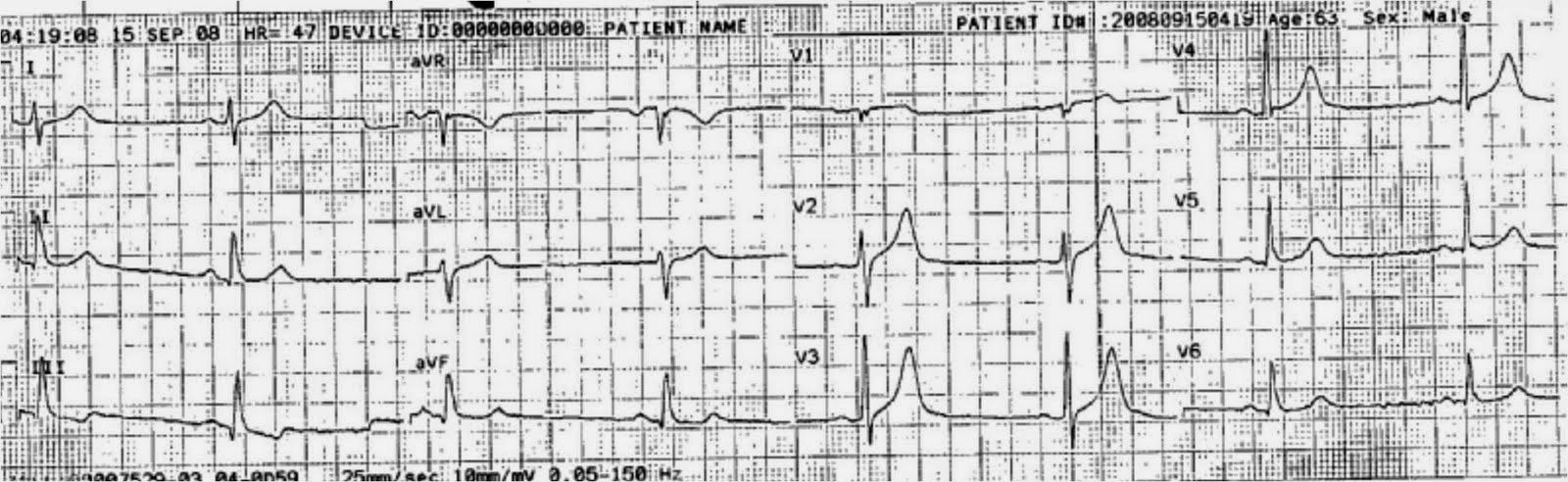
ECG 2.5 hours after presentation, no therapy other than aspirin:
 |
| The terminal T-wave invesions are still present and perhaps more noticeable. |
At this point, the troponin returned at 0.14 ng/ml (limit of detection: 0.012; 99% reference value: 0.034, so this is a “positive”).
Here is a third ED ECG at 6 hours:
 |
| The terminal T-wave inversions in V2-V4 are more obvious. This is typical of Wellens’ pattern A. |
The K was also 2.9 mEq/L, but this does not account for the ECG findings. The patient had a negative PE workup and was admitted to the hospital. She had a rise and fall of troponin, with a peak at 0.358 ng/ml. She went for an angiogram the next AM; it showed mid-LAD culprit lesion with 95% stenosis and was stented.
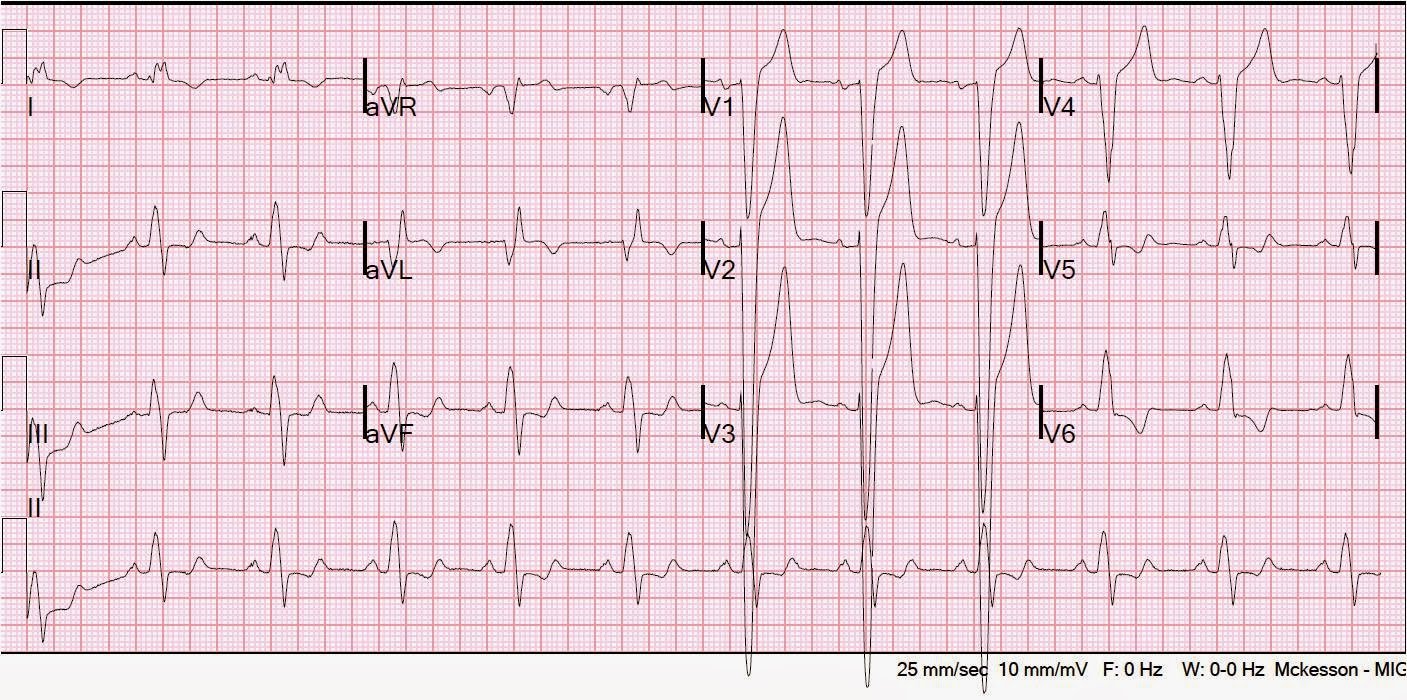
This is after LAD stenting:
 |
| After stenting, there was another rise and fall of troponin. Now the Pattern A Wellens’ waves are very well developed. |
T-wave inversion in LAD ACS:
Wellens’ syndrome is chest pain that is relieved with terminal T-wave inversion on the initial, pain-free, ECG. There is preservation of R-waves, and there is evolution to deeper T-wave inversion (Wellens’ Pattern B). It is due to brief LAD occlusion with reperfusion. This last evolution (Pattern B) did not occur in this case.
See here for a series of classic Wellens’ evolution over 26 hours.