See our newest OMI publication in JEM
Free full text here:
https://authors.elsevier.com/
Comparison of the ST-elevation myocardial infarction (STEMI) vs. NSTEMI and Occlusion MI (OMI) vs. NOMI paradigms of acute MI
Background: The current ST-elevation
myocardial infarction (STEMI) vs. non-STEMI (NSTEMI)
paradigm prevents some NSTEMI patients with acute coronary occlusion from receiving emergent reperfusion, in spite
of their known increased mortality compared with NSTEMI
without occlusion. We have proposed a new paradigm
known as occlusion MI vs. nonocclusion MI (OMI vs.
NOMI).
Objective: We aimed to compare the two paradigms
within a single population. We hypothesized that STEMI(–)
OMI would have characteristics similar to STEMI(+) OMI
but longer time to catheterization.
Methods: We performed
a retrospective review of a prospectively collected acute coronary syndrome population. OMI was defined as an acute
culprit and either TIMI 0–2 flow or TIMI 3 flow plus peak
troponin T greater than or equal to 1.0 ng/mL. We collected electrocardiograms,
demographic characteristics, laboratory results, angiographic data, and outcomes.
Results: Among 467 patients,
there were 108 OMIs, with only 60% (67 of 108) meeting
STEMI criteria. Median peak troponin T for the STEMI(+)
OMI, STEMI(–) OMI, and no occlusion groups were 3.78
(interquartile range [IQR] 2.18–7.63), 1.87 (IQR 1.12–
5.48), and 0.00 (IQR 0.00–0.08). Median time from arrival
to catheterization was 41 min (IQR 23–86 min) for
STEMI(+) OMI compared with 437 min (IQR 85–
1590 min) for STEMI(–) OMI (p less than 0.001). STEMI(+) OMI
was more likely than STEMI(–) OMI to undergo catheterization within 90 min (76% vs. 28%; p less than 0.001).
Conclusions:
STEMI(–) OMI patients had significant delays to catheterization but adverse outcomes more similar to STEMI(+)
OMI than those with no occlusion. These data support the
OMI/NOMI paradigm and the importance of further
research into emergent reperfusion for STEMI(–)
OMI.
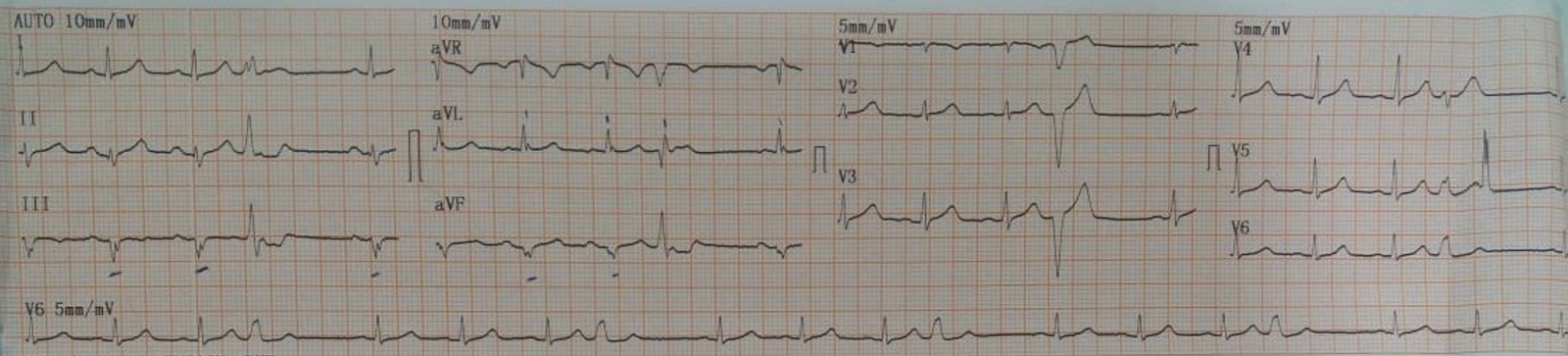
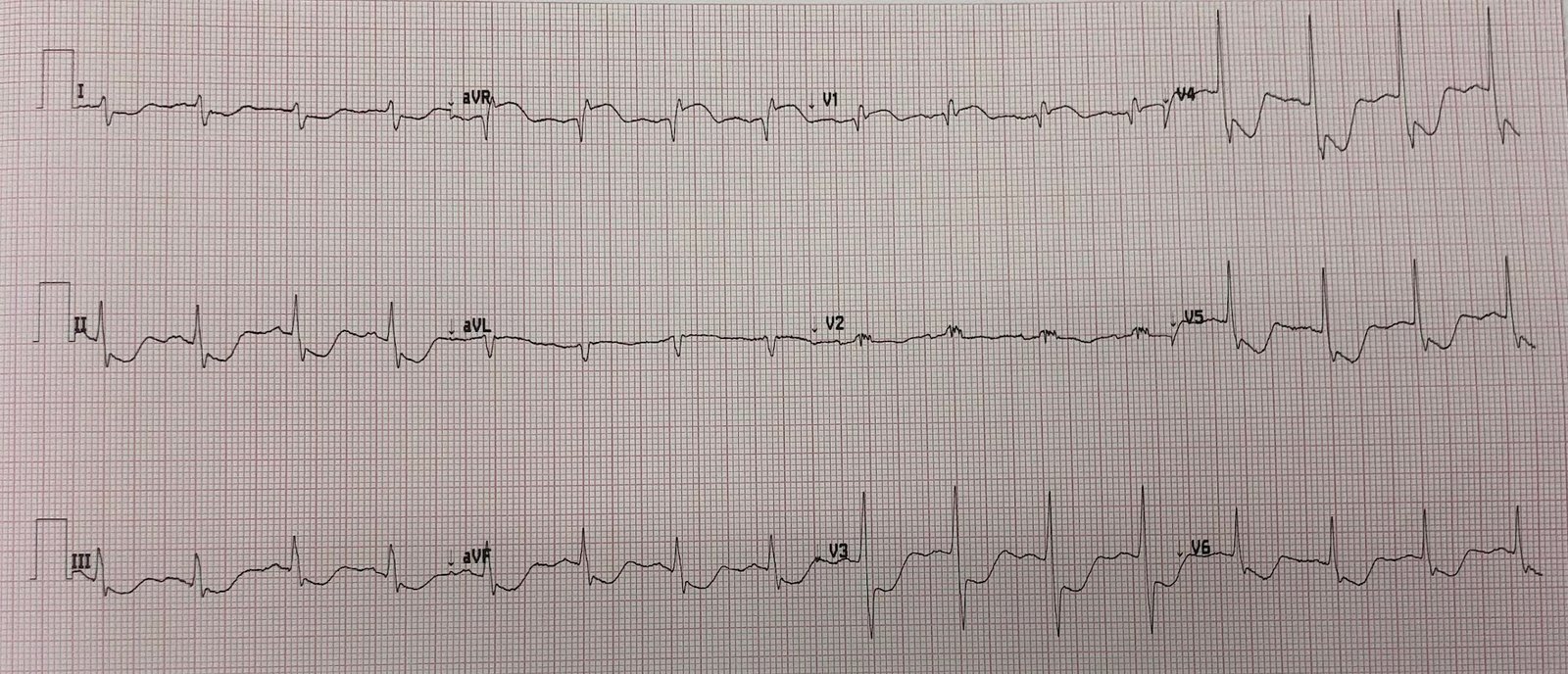
If your understanding of ACS stops at the STEMI vs. NSTEMI concept, then this figure below appears at first glance to justify and summarize your practice:
But in reality, the paradigm keeps an important population hidden from your understanding: the NSTEMI patients with OMI. Their peak troponins were similar to the obvious STEMIs, and of course they both have OMI.