If you are giving tPA to patients with STEMI, it is wise to avoid IV nitroglycerine. I am revisiting this topic because of a recent case I posted in which a patient who was on IV nitro received tPA. This patient was very hypertensive, and thus needed something to control BP. But I would advise against nitroglycerine.
This is data that very few cardiologists are aware of
Background:
First, know that, in the reperfusion era, there is absolutely no data to support the use of nitroglycerine in STEMI. See the ACC/AHA recommendation below that puts the level of evidence at “C”. I have pasted below the ACC/AHA guideline. There are a total of 4 references provided. Three are from the pre-reperfusion era (1 shows is a pooled analysis showing decrease in mortality from 7.7% to 7.4%); 1 uses transdermal nitrates.
There is data showing worse outcome with nitroglycerine when tPA is used (see 3 abstracts pasted below, one is a randomized human study, though small). This data is far better than that referenced in the guidelines, and actually also includes rationale and lab confirmation (tPA levels are much lower with, than without, nitro drips).
The reason for this is that Nitro apparently increases hepatic blood flow and tPA metabolism, lowering tPA blood levels.
Some have argued that GISSI-3 proved nitro to be efficacious. This simply shows a bias towards nitro and away from any data about it. GISSI-3 studied transdermal nitrates, given all day for 6 weeks. Furthermore, and I quote from the article: “the systematic administration of transdermal GTN did not show any independent effect on the outcome measures (0.94 [0.84-1.05] and 0.94 [0.87-1.02]).”
The application of literature that is prior to the thrombolytic and even aspirin era to the reperfusion era of today is not rational.
With the evidence below, and at least one other study (White CM. Pharmacotherapy 20(4):380-2, April 2000) confirming decrease in tPA levels with use of nitro, it would be very unwise to give nitrates and expect tPA to work.
Even with HTN or pulmonary edema, I would use another drug if I were giving tPA and expecting reperfusion. Exactly which medication would be better, however, is uncertain. Beta blockers probably do not have this effect on tPA, but some other vasodilators (if beta blockade does not sufficiently lower the BP) might also have this effect. IV enalapril is one possibility, but can have irreversible hypotensive effects. Nitroprusside is great to lower BP, but does it also lower tPA levels? In any case, I would try beta blockade first if there are no absolute contraindications. The BP must be less than 185/110 in order to give tPA and avoid catastrophic intracranial bleeding.
Finally, the dose used that interrupted reperfusion was high (100 mcg/min), but any efficacious dose of nitro would have to be high (many physicians forget that sublingual nitro q 5 minutes is equal to 80 mcg/min).
tPA and Nitroglycerine: an Annotated Bibliography:
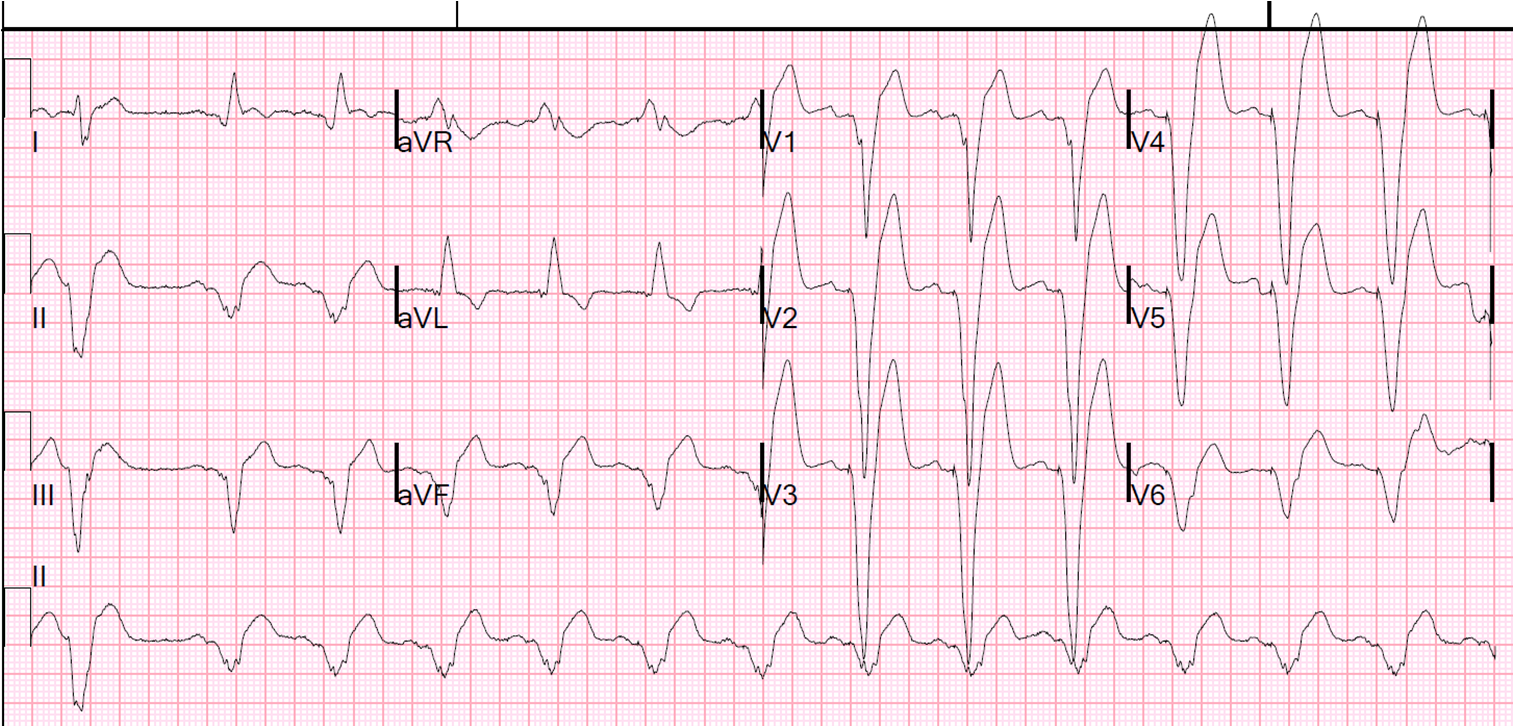
Concurrent nitroglycerine therapy impairs tissue-type plasminogen activator-induced thrombolysis in patients with acute myocardial infarction.1
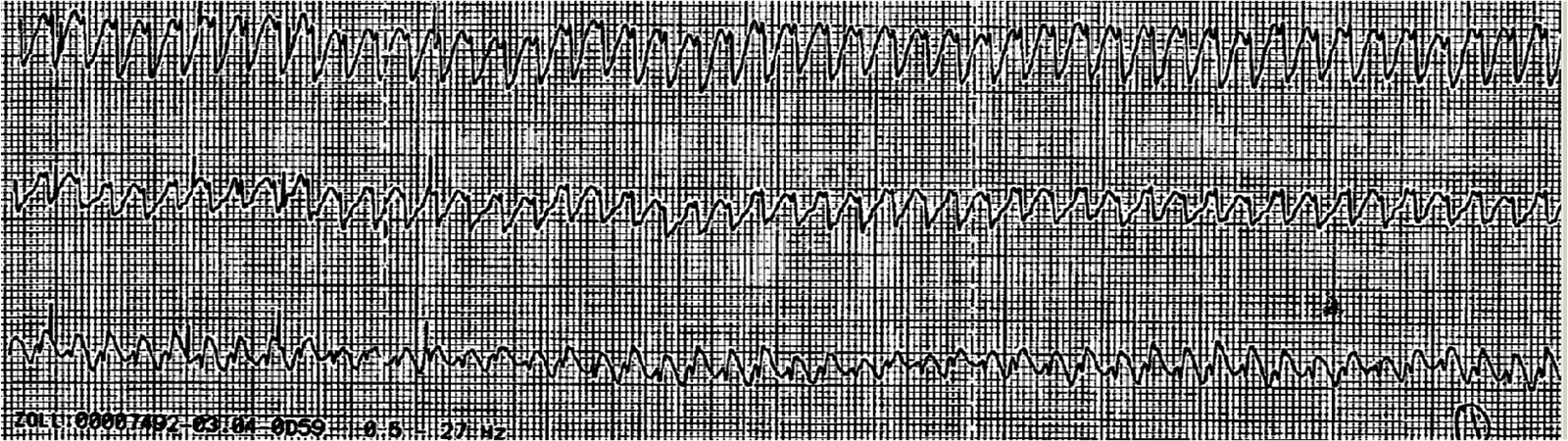
Nitroglycerin given with tissue-type plasminogen activator (t-PA) has been shown to decrease the thrombolytic effect of t-PA in animal models of coronary artery thrombosis. The present study was conducted to determine whether such an interaction between nitroglycerin and t-PA occurs in patients with acute myocardial infarction undergoing thrombolytic treatment. Patients with acute myocardial infarction were treated with t-PA plus saline solution (group 1; n = 11) or t-PA plus nitroglycerin (group 2; n = 36). Stable coronary artery reperfusion assessed by continuous ST-segment monitoring in 2 electrocardiographic leads, and release of creatine kinase occurred in 91% of group 1 patients and in 44% of group 2 patients (95% confidence interval, 14% to 82%; p < 0.02). Plasma levels of t-PA antigen were consistently (p < 0.005) higher in group 1 than in group 2 patients up to 6 hours after t-PA infusion. Conversely, plasminogen activator inhibitor-1 (PAI-1) levels were slightly higher in group 2 than in group 1 patients. These observations indicate that nitroglycerin given with t-PA significantly decreases the plasma t-PA antigen concentrations and impairs the thrombolytic effect of t-PA in patients with acute myocardial infarction.
Concurrent nitroglycerine administration decreases thrombolytic potential of tissue-type plasminogen activator.2
Dynamic coronary vasoconstriction may play a role in coronary artery reocclusion after successful thrombolysis. The effect of nitroglycerin on the thrombolytic effects of recombinant tissue-type plasminogen activator (rt-PA) was examined in dogs with an electrically induced occlusive coronary artery thrombus. Eleven dogs were randomly given rt-PA alone and seven rt-PA with nitroglycerin. The dose of rt-PA was 0.75 mg/kg body weight given over 20 min and the dose of nitroglycerin was 125 micrograms/min for 40 min. The reperfusion rate in the dogs given rt-PA alone was 73% (8 of 11 dogs) and that in the rt-PA plus nitroglycerin group was 57% (four of seven dogs) (p = NS). The time to thrombolysis (or reperfusion) in dogs receiving rt-PA plus nitroglycerin was 70% greater than in those receiving rt-PA alone (means +/- SD/29.8 +/- 9.9 versus 17.6 +/- 5.9 min, p less than 0.02), and the duration of reperfusion much shorter (11 +/- 17 versus 42 +/- 16 min, p less than 0.02). Peak coronary blood flow after reperfusion in dogs receiving rt-PA plus nitroglycerin was also less than in those receiving rt-PA alone (36 +/- 52 versus 63 +/- 20 ml/min, p less than 0.02). Reocclusion occurred in all dogs given rt-PA with nitroglycerin and in six of eight given rt-PA alone (p = NS). Plasma concentrations of rt-PA were lower when nitroglycerin was given with rt-PA alone (427 +/- 279 versus 1,471 +/- 600 ng/ml, p less than 0.01).
administration of rt-PA alone, but not with administration of rt-PA with
nitroglycerin (0.23 ± 0.57 and 5.26 ± 6.23, respectively, p less than 0.02).
Peripheral blood platelet count decreased during thrombus formation in all dogs;
with administration of rt-PA alone, platelet counts stabilized but continued to
decrease with concurrent administration of nitroglycerin with rt-PA (mean
platelet counts at the end of rt-PA infusion 7.23 ± 1.68 and 4.78 ± 3.00 ×
108/ml, respectively, p less than 0.02), suggesting
continued sequestration of platelets in the intracoronary thrombus. In four
additional dogs nitroglycerin was given after rt-PA-induced thrombolysis, but
nitroglycerin failed to sustain coronary artery reperfusion.This study shows that 1) nitroglycerin given concurrently with
rt-PA may have a detrimental effect on the thrombolytic potential of rt-PA,
probably because of the reduction in plasma t-PA concentrations, and 2)
nitroglycerin given after rt-PA-induced thrombolysis does not prevent coronary
artery reocclusion.
Concurrent nitroglycerin administration reduces the efficacy of recombinant tissue-type plasminogen activator in patients with acute anterior wall myocardial infarction.3
The aim of this study was to evaluate the impact of concurrent nitroglycerin administration on the thrombolytic efficacy of recombinant tissue-type plasminogen activator (rTPA) in patients with acute anterior myocardial infarction (AMI). Sixty patients (53 men, 7 women; mean age 54 +/- 7 years) with AMI entered the study. Thirty-three patients were randomized to receive rTPA alone (100 mg in 3 hours) (group A) and 27 to receive rTPA plus nitroglycerin (100 micrograms/min) (group B). Time from the onset of chest pain and delivery of rTPA was similar in the two groups of patients. Patients in group A had signs of reperfusion more often than the patients in group B (25 of 33 or 75.7% vs 15 of 27 or 55.5%, p less than 0.05). Time to reperfusion was also shorter in group A than in group B (19.6 +/- 9.4 minutes vs 37.8 +/- 5.9 minutes, p less than 0.05). Group B had a greater incidence of in-hospital adverse events (9 of 27 vs 5 of 33, p less than 0.05) and a higher incidence of coronary artery reocclusion (8 of 15 or 53.3% vs 6 of 25 or 24%, p less than 0.05). Peak plasma levels of rTPA antigen were higher in group A compared with group B (1427 +/- 679 vs 512 +/- 312 ng/ml, p less than 0.01). In conclusion, concurrent nitroglycerin administration reduces the thrombolytic efficacy of rTPA in patients with AMI probably by lowering the plasma levels of rTPA antigen. The diminished efficacy of rTPA is associated with an adverse outcome.
References
1. Nicolini FA, Ferrini D, Ottani F, et al. Concurrent nitroglycerine therapy impairs tissue-type plasminogen activator-induced thrombolysis in patients with acute myocardial infarction. Am J Cardiol 1994; 74:662-666.
2. Mehta JL, Nicolini FA, Nichols WW, Saldeen TG. Concurrent nitroglycerine administration decreases thrombolytic potential of tissue-type plasminogen activator. J Am Coll Cardiol 1991; 17:805-811. Full text:
3. Romeo F, Rosano GM, Martuscelli E, et al. Concurrent nitroglycerin administration reduces the efficacy of recombinant tissue-type plasminogen activator in patients with acute anterior wall myocardial infarction. Am Heart J 1995; 130:692-697.
From ACC/AHA Guidelines
Class I
1. Patients with ongoing ischemic discomfort should receive sublingual nitroglycerin (0.4 mg) every 5 minutes for a total of 3 doses, after which an assessment should be made about the need for intravenous nitroglycerin.
(Level of Evidence: C)
2. Intravenous nitroglycerin is indicated for relief of ongoing ischemic discomfort, control of hypertension, or management of pulmonary congestion. (Level of
Evidence: C)
Class III
1. Nitrates should not be administered to patients with systolic blood pressure less than 90 mm Hg or greater than or equal to 30 mm Hg below baseline, severe bradycardia (less than 50 beats per minute [bpm]), tachycardia (more than 100 bpm), or suspected RV infarction. (Level of Evidence: C)
2. Nitrates should not be administered to patients who have received a phosphodiesterase inhibitor for erectile dysfunction within the last 24 hours (48 hours for tadalafil). (Level of Evidence: B)
The physiological effects of nitrates include reducing preload and afterload through peripheral arterial and venous
dilation, relaxation of epicardial coronary arteries to improve coronary flow, and dilation of collateral vessels, potentially creating a more favorable subendocardial to epicardial flow ratio (252-254). Vasodilation of the coronary arteries, especially at or adjacent to sites of recent plaque disruption, may be particularly beneficial for the patient with acute infarction. Nitrate-induced vasodilatation may also have particular utility in those rare patients with coronary spasm presenting as STEMI.
Clinical trial results have suggested only a modest benefit from nitroglycerin used acutely in STEMI and continued
subsequently. A pooled analysis of more than 80 000 patients treated with nitrate-like preparations intravenously or orally in 22 trials revealed a mortality rate of 7.7% in the control group, which was reduced to 7.4% in the nitrate group. These data are consistent with a possible small treatment effect of nitrates on mortality such that 3 to 4 fewer deaths would occur for every 1000 patients treated (152). Nitroglycerin may be administered to relieve ischemic pain and is clearly indicated as a vasodilator in patients with STEMI associated with
152. ISIS-4 (Fourth International Study of Infarct Survival) Collaborative Group. ISIS-4: a randomised factorial trial assessing early oral captopril, oral mononitrate, and intravenous magnesium sulphate in 58,050 patients with suspected acute myocardial infarction. Lancet1995;345:669-85.
252. Abrams J. Hemodynamic effects of nitroglycerin and long-acting nitrates. Am Heart J 1985;110:216-24. 253. Winbury MM. Redistribution of left ventricular blood flow produced by nitroglycerin: an example of integration of the macroand microcirculation. Circ Res 1971;28(Suppl 1):140-7.
254. Gorman MW, Sparks HV. Nitroglycerin causes vasodilatation within ischaemic myocardium. Cardiovasc Res 1980;14:515-21.


Is Nitroglycerin has the same effect on Streptokinase ?!!
I don't know of any data. Sorry.
What's your opinion on ntg in STEMI? Since there's no solid evidence the decrease in mortality is statistically significant, should we still give it? This is a frequently debated topic on social media.
Floyd,
There is no good evidence for risk or benefit (no randomized trials that I know of). I think it probably helps more than hurts and so I would give it as long as the BP can handle it.
Steve